- Sarcoidosis: May be bilateral. Typically painless. May have concomitant lung, skin, or renal disease. Lymphadenopathy, parotid gland enlargement, or seventh cranial nerve palsy may be present. Of note, intraocular involvement is uncommon in patients with adnexal sarcoidal inflammation, and vice versa. More common in Americans of African descent, West Africans, and Northern Europeans.
- IOIS: See 7.2.2, IDIOPATHIC ORBITAL INFLAMMATORY SYNDROME. Chronic, painless lacrimal gland enlargement is possible, but atypical for IOIS.
- IgG4-related dacryoadenitis. See NOTE in 7.2.2, IGG4-RELATED ORBITOPATHY.
- Infectious: Enlarged palpebral lobe with surrounding conjunctival injection. Purulent discharge with bacterial dacryoadenitis, which is much less common than noninfectious dacryoadenitis. Bilateral lacrimal gland enlargement may be seen in patients with viral illnesses. CT scan may show fat stranding, abscess.
- Benign mixed tumor (pleomorphic adenoma): Slowly progressive, painless proptosis or inferomedial displacement of the globe in middle-aged adults. Usually involves the orbital lobe of the lacrimal gland. CT may show a well-circumscribed mass with pressure-induced remodeling and enlargement of the lacrimal gland fossa. No true bony erosion occurs (Figure 7.6.1A).
- Lymphoproliferative tumor: Slowly progressive proptosis and globe displacement in an adult. May have a pink “salmon-patch” area of subconjunctival extension. CT usually shows a lacrimal gland lesion that conforms to the native anatomy and is well circumscribed. Indolent forms spare the bone, but bony erosion may be seen in aggressive histopathology (e.g., diffuse large B-cell and mantle cell lymphoma) (Figure 7.6.1C).
- ACC: Subacute onset of pain over 1 to 3 months, proptosis, and diplopia, with variable progression. Globe displacement, ptosis, and a motility disturbance are common. This malignant lesion often exhibits perineural invasion, resulting in pain along the temple or forehead and intracranial extension. CT shows an irregular mass, often with bony erosion (Figure 7.6.1B).
- Malignant mixed epithelial tumor (pleomorphic adenocarcinoma): Occurs primarily in elderly patients, acutely producing pain and progressing rapidly. May develop primarily or secondarily within a long-standing benign mixed epithelial tumor (“carcinoma ex pleomorphic adenoma”), or incompletely resected benign mixed tumor. CT findings are similar to those for ACC.
- Lacrimal gland cyst (dacryops): Usually an asymptomatic mass that may fluctuate in size. Typically occurs in a young adult or middle-aged patient.
- Others (may not involve the lacrimal gland, but occur superolaterally in the area of the lacrimal gland and fossa): GPA (formerly Wegener granulomatosis), tuberculosis, leukemia, mumps, mononucleosis, syphilis (exceedingly rare), mucoepidermoid carcinoma, plasmacytoma/multiple myeloma, eosinophilic granuloma, metastasis (especially prostate adenocarcinoma), and dermoid cyst (Figure 7.6.1D) (see Tables 7.4.1.2 and
14.3.2
).
7-6.1 CT and MRI of lesions involving or near the lacrimal gland.
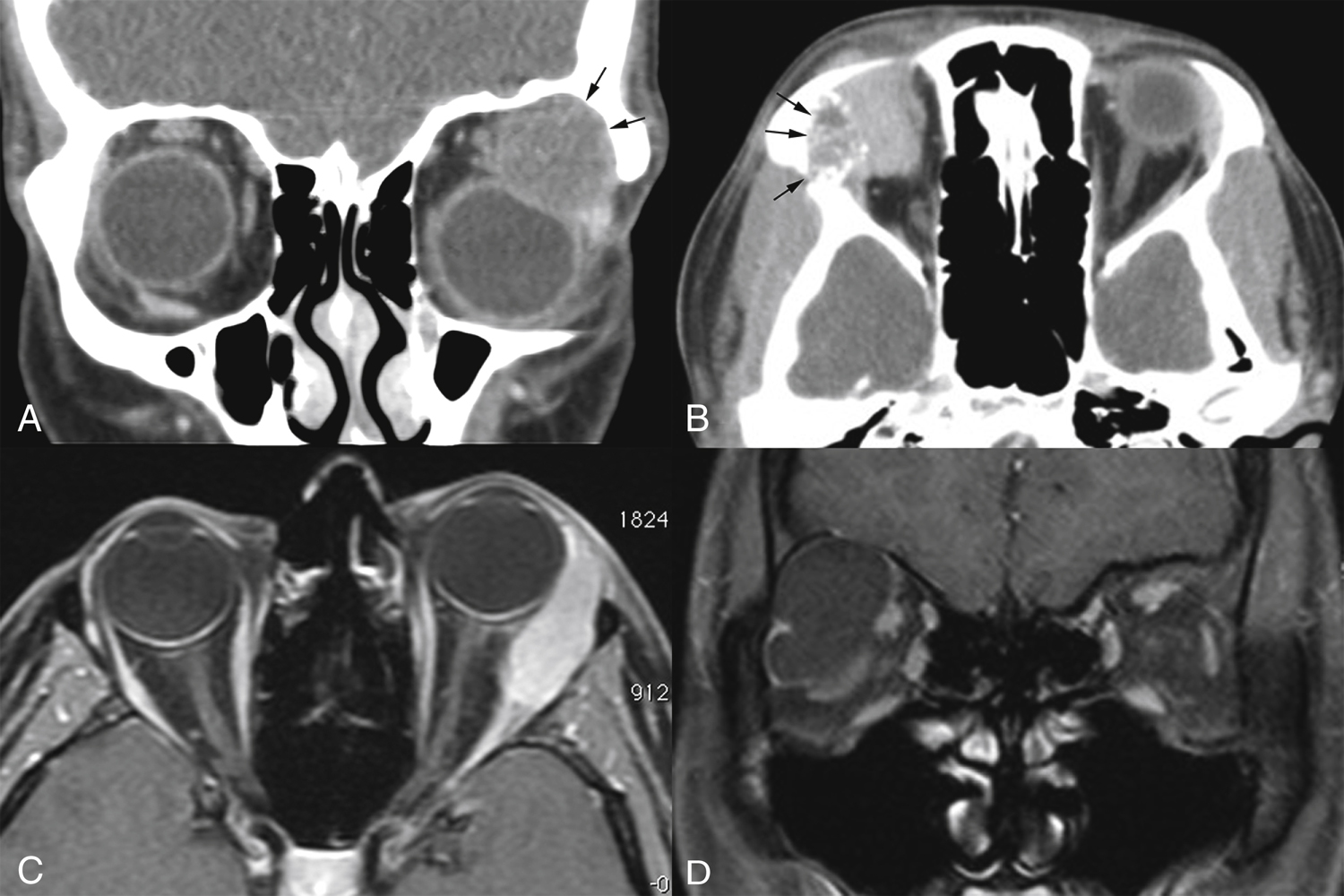
A:Pleomorphic adenoma with smooth, pressure induced changes in the lacrimal gland fossa (arrows).B:Adenoid cystic carcinoma with bone destruction (arrows) and intralesional calcifications.C:Lymphoma involving the lacrimal gland with molding to the globe.D:Dermoid cyst arising from the frontoethmoidal suture.
Primary, epithelial neoplasms are almost always unilateral; inflammatory disease may be bilateral. Lymphoma is more commonly unilateral, but may be bilateral. |