Pain, photophobia, red eye, foreign body sensation, and mildly decreased vision.
(See Figure 4.1.1.)
Critical
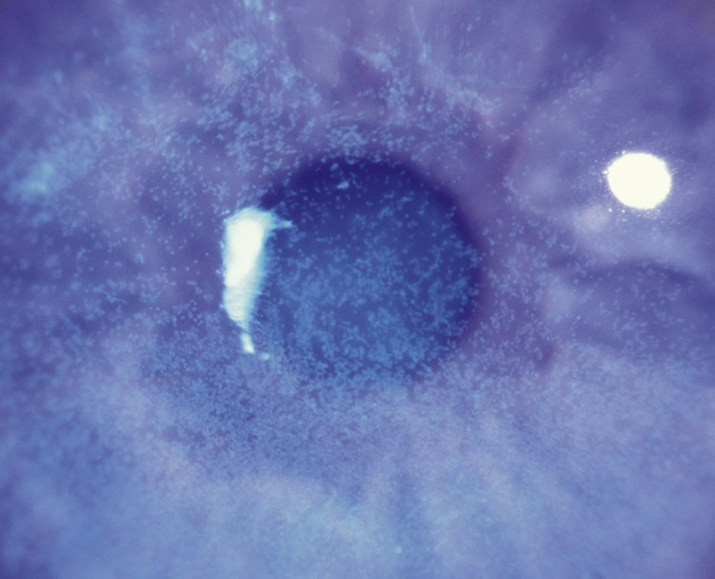
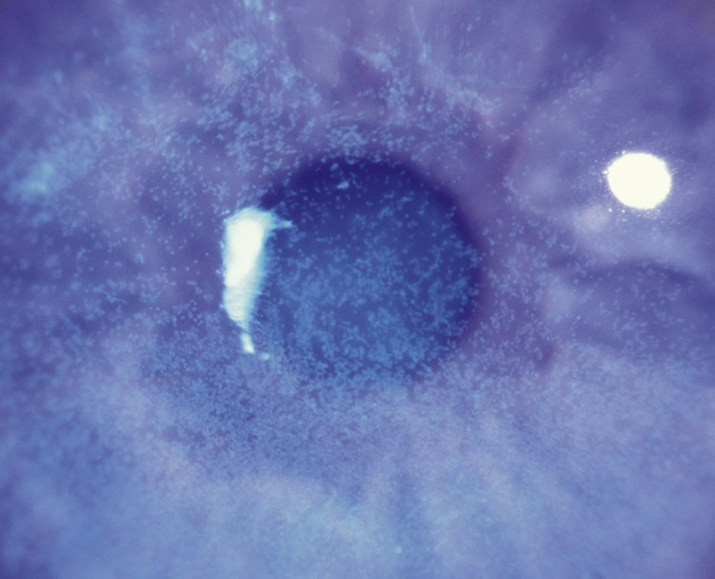
Pinpoint locations of corneal epithelial cell damage or breakdown that stain with fluorescein. May be confluent if severe. Staining pattern may allude to etiology. Pain is relieved by the instillation of anesthetic drops. Also referred to as punctate epithelial erosions.
 NOTE: NOTE: |
Relief of pain with the instillation of anesthetic drops (e.g., proparacaine) strongly suggests corneal epithelial disease as the etiology of pain. Although anesthetic drop instillation is an essential part of the ocular examination, patients should NEVER be prescribed topical anesthetic drops, and the clinician should ensure the patient does not take anesthetic drops from the office. When used chronically, these drops inhibit epithelial healing and may cause corneal ulceration. |
Other
Conjunctival injection and watery discharge.
4-1.1 Superficial punctate keratopathy stained with fluorescein.
Superficial punctate keratopathy (SPK) is nonspecific but is most commonly seen in the following disorders, which may be associated with a specific staining pattern:
- Superior staining
- Contact lens–related disorder (e.g., chemical toxicity, tight lens syndrome, contact lens overwear syndrome, giant papillary conjunctivitis). See 4.20, CONTACT LENS-RELATED PROBLEMS.
- Foreign body under the upper eyelid: Typically linear SPK, fine epithelial defects arranged vertically.
- Floppy eyelid syndrome: Extremely loose upper eyelids that evert easily. See 6.6, FLOPPY EYELID SYNDROME.
- Superior limbic keratoconjunctivitis (SLK): Superior bulbar conjunctival inflammation. See 5.4, SUPERIOR LIMBIC KERATOCONJUNCTIVITIS.
- Vernal conjunctivitis: Atopy, large conjunctival papillae under the upper eyelid and/or limbus. See 5.1, ACUTE CONJUNCTIVITIS.
- Interpalpebral staining
- Inferior staining
- Blepharitis: Erythema, telangiectasias, or crusting of the eyelid margins, meibomian gland dysfunction. See 5.8, BLEPHARITIS/MEIBOMITIS.
- Exposure keratopathy: Poor eyelid closure with failure of eyelids to cover the entire globe. See 4.5, EXPOSURE KERATOPATHY.
- Topical drug toxicity (e.g., neomycin, gentamicin, trifluridine, atropine, as well as any drop with preservatives, including artificial tears, or any frequently used drop).
- Conjunctivitis: Discharge, conjunctival injection, and eyelids stuck together on awakening. See 5.1, ACUTE CONJUNCTIVITIS and 5.2, CHRONIC CONJUNCTIVITIS.
- Trichiasis/distichiasis: One or more eyelashes rubbing against the cornea (superior SPK if misdirected lashes from upper eyelid). See 6.5, TRICHIASIS.
- Entropion or ectropion: Eyelid margin turned in or out (superior SPK if upper eyelid abnormality). See 6.3, ECTROPION and 6.4, ENTROPION.
- Other
- Trauma: SPK can occur from relatively mild trauma, such as chronic eye rubbing.
- Mild chemical injury: See 3.1, CHEMICAL BURN.
- Thygeson superficial punctate keratitis: Bilateral, recurrent epithelial keratitis (raised epithelial staining lesions, not micro erosions) without conjunctival injection. See 4.8, THYGESON SUPERFICIAL PUNCTATE KERATITIS.
See the appropriate section to treat the underlying disorder. SPK is often treated nonspecifically as follows:
- Noncontact lens wearer with a small amount of SPK
- Artificial tears q.i.d., preferably preservative-free.
- Can add a lubricating gel or ointment q.h.s.
- Noncontact lens wearer with a large amount of SPK
- Preservative-free artificial tears q2h.
- Ophthalmic antibiotic ointment (e.g., bacitracin/polymyxin B or erythromycin q.i.d. for 3 to 5 days).
- Consider a cycloplegic drop (e.g., cyclopentolate 1% t.i.d.) for relief of pain and photophobia.
- Contact lens wearer with a small amount of SPK
- Discontinue contact lens wear.
- Artificial tears q.i.d., preferably preservative-free.
- Can add a lubricating gel or ointment q.h.s.
- Contact lens wearer with a large amount of SPK
- Discontinue contact lens wear.
- Antibiotic: Fluoroquinolone (e.g., ciprofloxacin, gatifloxacin, moxifloxacin, or besifloxacin) or aminoglycoside (e.g., tobramycin) drops four to six times per day as well as ophthalmic ointment q.h.s. (e.g., ciprofloxacin or bacitracin/polymyxin B). If confluent SPK, consider ophthalmic antibiotic ointment four to six times per day.
- Consider a cycloplegic drop (e.g., cyclopentolate 1% t.i.d.) for relief of pain and photophobia.
 NOTE: NOTE: |
DO NOT patch contact lens–related SPK or epithelial defects because they can quickly develop into severely infected ulcers. |