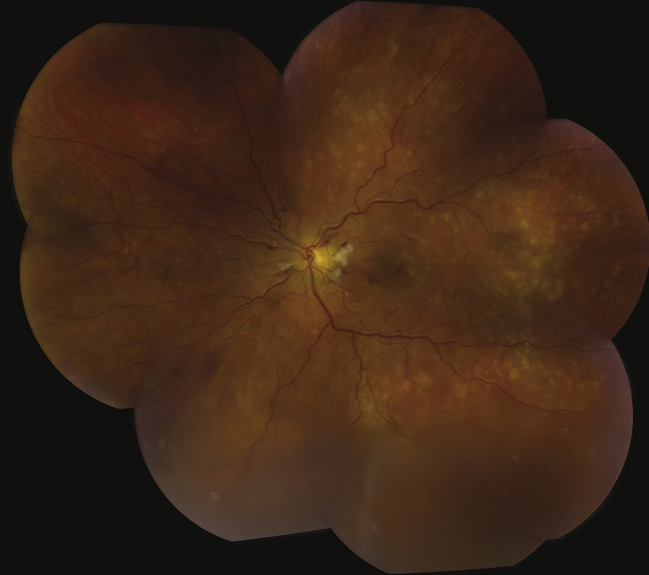
(See Figure 11.10.1.)
Critical
Generalized or localized retinal arteriolar narrowing, almost always bilateral.
Other
- Chronic HTN: Arteriovenous crossing changes (“AV nicking”), retinal arteriolar sclerosis (“copper” or “silver” wiring), CWSs, flame-shaped hemorrhages, arterial macroaneurysms, central or branch occlusion of an artery or vein. Rarely, neovascular complications can develop.
- Acute (“malignant”) HTN or accelerated HTN: Hard exudates often in a “macular star” configuration, retinal edema, CWSs, flame-shaped hemorrhages, optic nerve head edema. Rarely serous RD or VH. Areas of focal chorioretinal atrophy (from previous choroidal infarcts [Elschnig spots]) are a sign of past episodes of acute HTN.
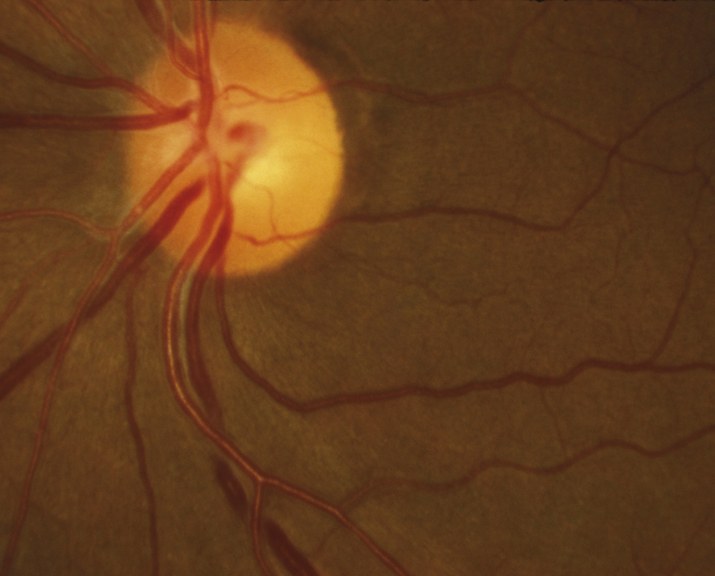
(See Figure 11.10.2.)
When unilateral, suspect carotid artery obstruction on the side of the normal-appearing eye, sparing the retina from the effects of the HTN. |