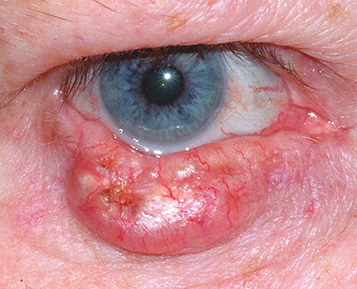
Basal cell carcinoma: Most common malignant eyelid tumor, often present in the medial canthus or the lower eyelid in middle-aged or elderly patients. Rarely metastasizes, but may be locally invasive, particularly when present in the medial canthal region. There are two major forms:
Nodular: Indurated, firm mass, commonly with telangiectasias over tumor margins (see Figure 6.8.1).
Infiltrative: The classic variant of this form is the morpheaform lesion. A firm, flat, subcutaneous lesion with indistinct borders. More difficult to excise due to the lack of visibly discrete margins, and may result in a large eyelid defect.
Squamous cell carcinoma (SCC): Variable presentation, may appear clinically similar to basal cell carcinoma. Regional metastasis may occur and can be extensive with the propensity for perineural invasion. A premalignant lesion, actinic keratosis, may appear either as a scaly, erythematous flat lesion or as a cutaneous horn, and can progress to SCC.
Keratoacanthoma: This lesion was previously considered to be benign and self-limiting; however, it is now regarded as a low-grade SCC. Clinically may resemble basal and SCCs. Typically, the lesion is elevated with rolled margins and a large central ulcer filled with keratin. Rapid growth with slow regression and even spontaneous resolution has been observed. Lesions usually involve the lower eyelid and can be destructive. Complete excision is recommended.
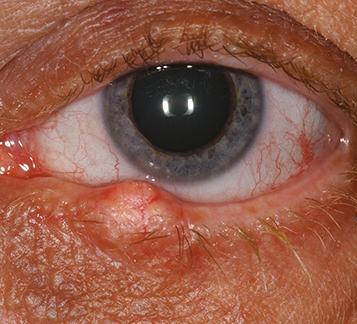
Sebaceous carcinoma: More common in middle-aged or elderly patients, usually elderly women. Most common on the upper eyelid but may be multifocal, involving both the upper and the lower eyelids. Often mistaken for a recurrent chalazion or intractable blepharitis. Loss of eyelashes and destruction of the meibomian gland orifices in the region of the tumor may occur. Regional and systemic metastasis or orbital extension is possible. Can occur many decades after prior radiation exposure to the eyelids (see Figure 6.8.2).
Others: Malignant melanoma, lymphoma, sweat gland carcinoma, metastasis (usually breast or lung), Merkel cell tumor, Kaposi sarcoma, and others.