Definition
Ophthalmoplegia secondary to lesion in the medial longitudinal fasciculus (MLF).
Double vision, blurry vision, or vague visual complaints.
(See Figures 10.13.1 and 10.13.2. See Video: Internuclear Ophthalmoplegia.)
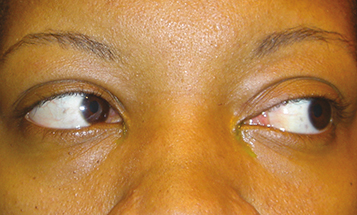
Figure 10.13.1: Left internuclear ophthalmoplegia: Left gaze showing full abduction.
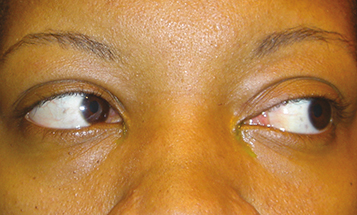
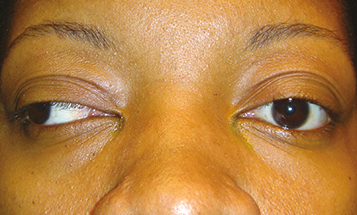
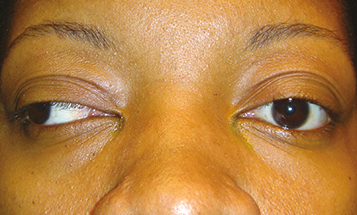
Figure 10.13.2: Left internuclear ophthalmoplegia: Right gaze with severe adduction deficit.
Critical
Weakness or paralysis of adduction, with horizontal jerk nystagmus of the abducting eye.
|
 NOTE NOTEINO is localized to the side with the weak adduction. |
Other
May be unilateral or bilateral (“wall-eyed” bilateral INO [WEBINO]). Upbeat nystagmus on upgaze may occur when INO is unilateral or bilateral. The involved eye can sometimes turn in when attempting to read (intact convergence). A skew deviation (relatively comitant vertical deviation not caused by neuromuscular junction disease or intraorbital pathology) may be present; brainstem and posterior fossa pathology should be ruled out. With skew deviation, the three-step test cannot isolate a specific muscle. See 10.7, Isolated Fourth Cranial Nerve Palsy. In addition, presence of other neurologic signs, including gaze-evoked nystagmus, gaze palsy, dysarthria, ataxia, and hemiplegia, favors skew deviation rather than fourth cranial nerve palsy.
Differential Diagnosis of Attenuated Adduction
Myasthenia gravis: May closely mimic INO; however, ptosis and orbicularis oculi weakness are common. Nystagmus of INO is faster; myasthenia gravis is more gaze paretic. Symptoms vary throughout the day.
Orbital disease (e.g., tumor, thyroid disease, idiopathic orbital inflammatory syndrome): Proptosis, globe displacement, or pain may be present. Nystagmus is usually not present. See 7.1, Orbital Disease.
One-and-a-half syndrome: Pontine lesion that includes the ipsilateral MLF and horizontal gaze center (sixth cranial nerve nucleus). The only preserved horizontal movement is abduction of the eye contralateral to the lesion. This is because of an ipsilateral adduction deficit (from the MLF lesion) and a horizontal gaze paresis in the direction of the lesion (from the horizontal gaze center lesion). Causes include stroke and pontine neoplasia.