Binocular vertical (or oblique) diplopia, difficulty reading, sensation that objects appear tilted; may be asymptomatic.
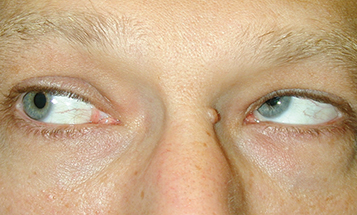
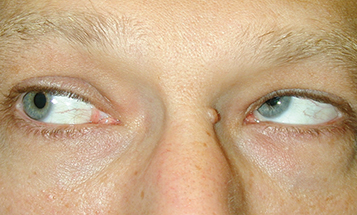
(See Figures 10.7.1 and 10.7.2. See Video: Fourth Cranial Nerve Palsy.)
Figure 10.7.1: Isolated left fourth cranial nerve palsy: Primary gaze showing left hypertropia.

Figure 10.7.2: Isolated left fourth cranial nerve palsy: Right gaze with left inferior oblique overaction.
Critical
Deficient inferior movement of an eye when attempting to look down and in. The three-step test isolates a palsy of the superior oblique muscle (see #3 under Workup, Perform the three-step test).
Other
The involved eye is higher (hypertropic) in primary gaze. The hypertropia increases when looking in the direction of the uninvolved eye or tilting the head toward the ipsilateral shoulder. The patient often maintains a head tilt toward the contralateral shoulder to eliminate diplopia.
All of the following may produce binocular vertical diplopia, hypertropia, or both:
Myasthenia gravis: Variable symptoms with fatigability. Ptosis common. Orbicularis oculi weakness often present. See 10.11, myasthenia gravis.
Thyroid eye disease: May have proptosis, eyelid lag, eyelid retraction, or injection over the involved rectus muscles. Positive forced duction test. See 7.2.1, Thyroid Eye Disease and Appendix 6, Forced Duction Test and Active Force Generation Test.
Idiopathic orbital inflammatory syndrome: Pain and proptosis are common. See 7.2.2, Idiopathic Orbital Inflammatory Syndrome.
Orbital fracture: History of trauma. Positive forced duction test. See 3.19, Orbital Blowout Fracture.
Skew deviation: The three-step test does not isolate a particular muscle. Rule out a posterior fossa or brainstem lesion with neuroimaging. See 10.13, Internuclear Ophthalmoplegia.
Incomplete third cranial nerve palsy: Inability to look down and in, usually with adduction weakness. Intorsion on attempted downgaze. Three-step test does not isolate the superior oblique. See 10.5, Isolated Third Cranial Nerve Palsy.
Brown syndrome: Limitation of elevation in adduction due to restriction of superior oblique tendon. May be congenital or acquired (e.g., trauma, inflammation). Positive forced duction test. See 8.8, Strabismus Syndromes.
GCA: Extraocular muscle ischemia causing nonspecific motility deficits or neural ischemia mimicking a cranial nerve palsy. Age ≥55 years, usually associated with systemic symptoms. See 10.17, Arteritic Ischemic Optic Neuropathy (Giant Cell Arteritis).
More Common
Trauma, vascular infarct (often the result of underlying diabetes or hypertension), congenital, or demyelinating disease.
Rare
Tumor, hydrocephalus, aneurysm, GCA.