Can vary from foreign body sensation to severe ocular pain (often out of proportion to the early clinical findings), redness, decreased vision, tearing, and photophobia over a period of several weeks.
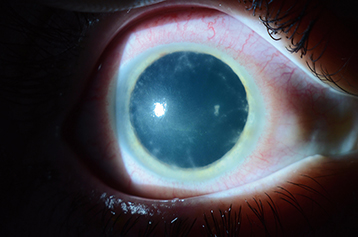
(See Figures 4.14.1 and 4.14.2.)
Figure 4.14.1: Acanthamoeba keratitis with radial keratoneuritis.
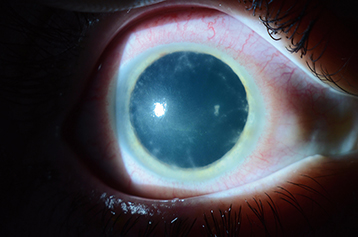
Figure 4.14.2: Acanthamoeba keratitis with a dense ring infiltrate.

Critical
Early: Epitheliitis with pseudodendrites, whorls, epithelial ridges, and/or diffuse subepithelial microcysts. Gray-white nonsuppurative subepithelial infiltrates (sometimes along corneal nerves, producing a radial keratoneuritis).
Late (3 to 8 weeks): Ring-shaped corneal stromal infiltrate; can become suppurative.
|
 NOTE NOTEAcanthamoeba keratitis should be considered in any patient with a history of contact lens wear, poor contact lens hygiene (e.g., using tap water to clean lenses, infrequent disinfection), and/or history of trauma or exposure to water (swimming, fishing, hot tub use) while wearing contact lenses. Although most patients with Acanthamoeba have a history of contact lens use, some patients do not and these patients often have a delayed diagnosis. Cultures for bacteria are negative (unless superinfection is present). The condition usually does not improve with antibiotic or antiviral medications and commonly follows a chronic, progressive, downhill course. Acanthamoeba is important to consider in patients with seemingly unresponsive HSV keratitis, as HSV keratitis usually responds well to appropriate treatment. The diagnosis of HSV keratitis in a contact lens wearer should always include consideration of Acanthamoeba, as the clinical appearance of these two entities can be similar in the early stages of disease. |
Other
Eyelid swelling, conjunctival injection (especially circumcorneal), cells and flare in the anterior chamber. Minimal discharge or corneal vascularization. Coinfection with bacteria or fungi may occur later in the course.
HSV keratitis is first in the differential. See 4.12, Bacterial Keratitis and 4.16, Herpes Simplex Virus.
See 4.12, Bacterial Keratitis for a general workup. One or more of the following are obtained when Acanthamoeba is suspected:
Corneal scrapings for Gram, Giemsa, calcofluor white, and periodic acid-Schiff stains (Giemsa and periodic acid-Schiff stains may show typical cysts). See Appendix 8, Corneal Culture Procedure.
Consider a culture on nonnutrient agar with Escherichia coli overlay.
Consider a corneal biopsy if the stains and cultures are negative and the condition is not improving on the current regimen.
Consider cultures and smears of contact lens and case.
IVCM may be helpful if available.
One or more of the following are usually used in combination, sometimes in the hospital initially:
Polyhexamethylene biguanide 0.02% (PHMB) drops q1h or chlorhexidine 0.02% drops q1h around the clock.
Propamidine isethionate 0.1% drops q1h are typically added in addition to PHMB 0.02% or chlorhexidine 0.02%. Dibromopropamidine isethionate 0.15% ointment is also available. Alternatively, PHMB 0.08% drops q1h can be used as single topical agent.
Consider an oral antifungal agent (e.g., itraconazole 400 mg p.o. for one loading dose, then 100 to 200 mg p.o. daily, ketoconazole 200 mg p.o. daily, or voriconazole 200 mg p.o. daily to b.i.d.).
All patients:
Miltefosine is designated by the United States Food and Drug Administration (FDA) as an orphan drug for the treatment of Acanthamoeba keratitis and can be considered as an adjunctive treatment to topical therapy. At Wills Eye, we typically begin this medication upon pathologic identification of Acanthamoeba cysts and prescribe 50 mg p.o. t.i.d. for a 4-week course. Treatment may extend up to 8 weeks in aggressive cases. Basic metabolic panel, liver function tests, and pregnancy test (if applicable) should be obtained prior to starting miltefosine, which is known to cause serious risks in pregnancy. Note that there may be rebound inflammation during the course of miltefosine or after it is stopped, which can respond to topical steroids.
Discontinue contact lens wear in both eyes.
Cycloplegic drop (e.g., cyclopentolate 1% t.i.d. or atropine 1% b.i.d.).
In the presence of inflammation, pain, and/or scleritis, oral nonsteroidal anti-inflammatory agents (e.g., naproxen 250 to 500 mg p.o. b.i.d.) may be used. Additional narcotic oral analgesics are often needed.
Topical steroids (e.g., prednisolone acetate 1% two to four times a day) may be used to improve symptoms after the initial ∼6 weeks of antiamoebic therapy.
|
 NOTE NOTEAlternative therapy includes hexamidine 0.1% drops, clotrimazole 1% drops, miconazole 1% drops, or paromomycin drops q2h. |
|
 NOTE NOTECorneal transplantation may be indicated for medical failures, but this procedure can be complicated by recurrent infection. It is best delayed for at least 6 to 12 months after medical treatment is completed. |
Every 1 to 4 days until the condition is consistently improving, and then every 1 to 4 weeks. Medication may then be tapered judiciously. Treatment is usually continued for 3 months after resolution of inflammation, which may take up to 6 to 12 months.
|
 NOTE NOTEPropamidine isethionate 0.1% drops are available in the United Kingdom and other countries; it may be compounded in the United States. PHMB is available in the United Kingdom as Cosmocil. It can be prepared by a compounding pharmacy in the United States from Baquacil, a swimming pool disinfectant.
|