Decreased vision, visual field defect, or asymptomatic; history of recent ocular trauma.
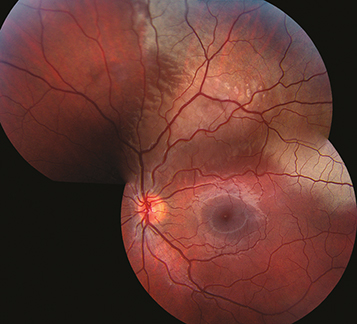
(See Figure 3.13.1.)
Confluent area of retinal whitening in the periphery or posterior pole. A cherry-red spot may be present. The retinal blood vessels are undisturbed in the area of retinal whitening.
Additional signs of ocular trauma, such as retinal hemorrhages, may be noted.
Blunt trauma to the globe causes shock waves which disrupt the photoreceptors. Retinal whitening is due to fragmentation of the photoreceptor outer segments (light scattering) and damage to the retinal pigment epithelium (RPE). The inner retinal layers may also be involved depending on the force of injury.
Retinal detachment: Retina elevated associated with retinal break or dialysis. See 11.3, Retinal Detachment.
Retinal artery occlusion: Retinal whitening along the distribution of an artery. See 11.6, Central Retinal Artery Occlusion and 11.7, Branch Retinal Artery Occlusion.
White without pressure: Common benign peripheral retinal finding. May be associated with a prominent vitreous base.
Myelinated nerve fiber layer: Develops postnatally (see Figure 11.5.2).
Chorioretinitis sclopetaria: Bare sclera visible through retinal and choroidal rupture on dilated examination. See 3.15, Chorioretinitis Sclopetaria.
Complete ophthalmic evaluation, including dilated fundus examination. See Video: Smartphone Video Indirect Ophthalmoscopy Guide. Scleral depression is performed except when a ruptured globe, hyphema, microhyphema, or iritis is present. See Video: Scleral Depression Tutorial. Optical coherence tomography (OCT) shows ellipsoid zone disruption.
No treatment is required because this condition is self-limited. Some patients with foveal involvement may be left with chronic visual impairment and RPE atrophy or hyperpigmentation.
Dilated fundus examination is repeated in 1 to 2 weeks. Patients are instructed to return sooner if retinal detachment symptoms are experienced (see 11.3, Retinal Detachment).