Decreased vision or asymptomatic. History of ocular trauma.
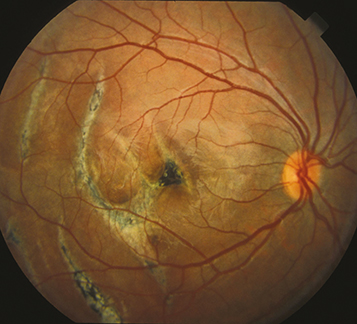
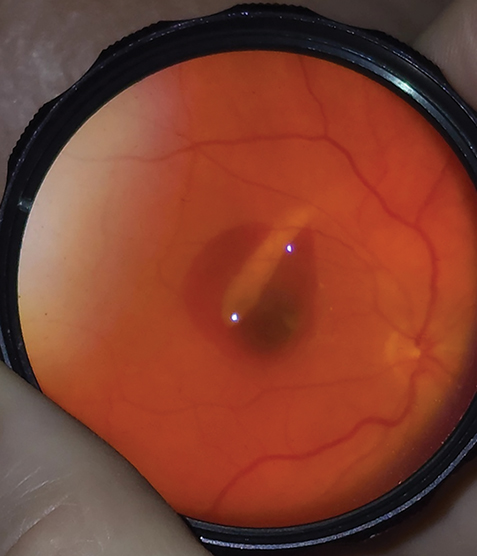
(See Figures 3.14.1 and 3.14.2.)
A yellow or white crescent-shaped subretinal streak, usually concentric to the optic disc (indirect injury) or in the peripheral fundus (direct injury). May be single or multiple. Often obscured for several days to weeks after inciting trauma due to overlying subretinal blood.
Rarely, the rupture may be radially oriented. Choroidal neovascularization (CNV) may develop later. Traumatic optic neuropathy (TON) may be present.
Lacquer cracks of high myopia: Often bilateral. A tilted disc, a scleral crescent adjacent to the disc, and a posterior staphyloma may also be seen. CNV may also develop in this condition. See 11.22, Pathologic/Degenerative Myopia.
Angioid streaks: Bilateral subretinal streaks radiating from the optic disc, sometimes associated with CNV. See 11.23, Angioid Streaks.
Complete ocular evaluation, including dilated fundus examination to rule out retinal breaks and to detect CNV.
Consider OCT and autofluorescence to characterize a choroidal rupture and evaluate potential CNV.
Consider fluorescein angiography to confirm the presence and location of CNV if the injury is old.
Observation. There are no medical or surgical treatment options in the acute setting. Consider recommending safety eyewear. An Amsler grid may be provided, and the patient is instructed to return if any change in the appearance of the grid is noted (see Appendix 4, Amsler Grid).
Anti–vascular endothelial growth factor (VEGF) therapy may be used if CNV develops. See 11.17, Neovascular or Exudative (Wet) Age-Related Macular Degeneration, for more information on CNV treatment.
After ocular trauma, patients with hemorrhage obscuring the underlying choroid are reevaluated every 1 to 2 weeks until the choroid can be well visualized. Although CNV is rare overall, ruptures that are particularly long or closer to the fovea are at greater risk for CNV development. Fundus examinations may be performed every 6 to 12 months depending on the severity and risk of progression to CNV. Patients treated for CNV must be followed closely after treatment to watch for persistent or new CNV (see 11.17, Neovascular or Exudative (Wet) Age-Related Macular Degeneration, for further follow-up guidelines).