Description
MRI uses a large magnetic field to excite protons in water. The energy given off as the protons re-equilibrate to their normal state is detected by specialized receivers (coils), which is then reconstructed into a two-dimensional or three-dimensional image.
Hospitals typically have machines with field strengths of 1.5 to 3 Tesla. In general, a stronger magnet allows better resolution or a faster scan at a lower resolution.
The basic principles of MRI are listed in Table 14.3.1. Figures 14.3.1 to 14.3.3 provide specific examples.
Figure 14.3.1: Axial T1-weighted image without fat suppression or gadolinium.
The vitreous is dark (hypointense) relative to the bright signal from fat. A well-circumscribed mass is clearly visible in the right orbit, also hypointense. Most orbital lesions are dark in T1 prior to gadolinium injection. The notable exceptions are listed in Table 14.3.2.

Figure 14.3.2: Axial T1 image with fat suppression and gadolinium of the patient seen in Figure 14.3.1.
Note how both the vitreous and fat are dark, but the extraocular muscles become bright. The orbital mass is now clearly visible. This technique should be performed in all orbital magnetic resonance imagings.

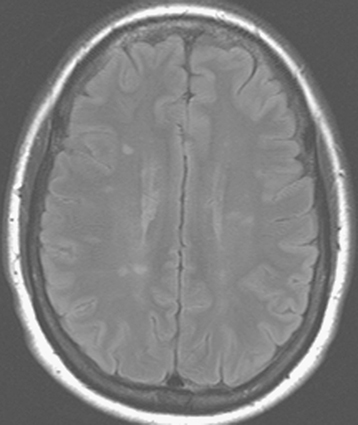
Figure 14.3.3: Axial T2-weighted image.
The vitreous is hyperintense (bright) relative to the orbital fat. The lesion seen in the prior two figures is also bright but in some cases may be isointense with the surrounding fat.
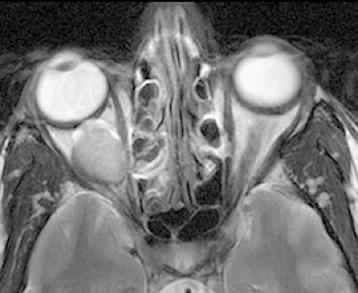
TABLE 14.3.1: Summary of Magnetic Resonance Imaging (MRI) Sequencesa
T1 Fat Suppression Gadolinium T2 Properties Useful for intraorbital structures such as optic nerve, extraocular muscles, and orbital vessels. The strong fat signal within the orbit gives poor resolution of lacrimal gland and may also mask intraocular structures. T1-weighted images with bright intraconal fat signal suppressed in the orbit, allowing for better anatomic detail. Essential for all orbital MRIs. Used with contrast (gadolinium). A paramagnetic agent that distributes in the extracellular space and does not cross the intact blood–brain barrier. Gadolinium is best for T1, fat-suppressed images. The lacrimal gland, extraocular muscles, and most orbital pathology enhance with gadolinium. Essential for all orbital MRIs. Always order with fat suppression in orbital studies. Suboptimal intraocular contrast. Demyelinating lesions (e.g., multiple sclerosis) are bright. The cerebrospinal fluid (CSF) signal may be useful in interpretation of optic nerve lesions/processes. Interpretation Fat is bright (high signal intensity). Vitreous and intracranial ventricles are dark. Vitreous and fat are dark. Extraocular muscles are bright. Most orbital masses are dark on T1 and become bright with gadolinium enhancement. Notable exceptions are listed in Table 14.3.2. Fluid-containing structures such as vitreous and CSF are bright. Melanin is dark.
FLAIR on T2 suppresses the bright signal from CSF and is especially helpful in identifying the periventricular lesions of demyelinating disease.a Note: High-flow areas create a dark area (“flow void”), which is helpful in identifying arterial structures (e.g., carotid siphon within the cavernous sinus).
Contrast studies can be ordered using gadolinium, a well-tolerated, non–iodine-based paramagnetic agent.
Diffusion-weighted imaging (DWI) is a technique that measures the Brownian motion of water within tissue. Lesions that are tightly packed by cells with a high nuclear to cytoplasmic ratio will minimize Brownian motion and “restrict diffusion.” DWI may help to distinguish highly cellular tumors (e.g., lymphoma) from inflammation. DWI is often coupled with an apparent diffusion coefficient (ADC) image, but the use of DWI/ADC in the orbit is limited. DWI can help differentiate the various phases of cerebral infarction (e.g., hyperacute, acute, subacute, and chronic).
Uses in Ophthalmology
Excellent for defining masses in the orbit and CNS. Signal-specific properties of certain pathology may be helpful in diagnosis (See Table 14.3.2).
TABLE 14.3.2: Tissues/Lesions That Appear Bright (Hyperintense) Relative to Vitreous on T1 Before Gadolinium Injectiona
Tissues/Lesions Examples Fat Lipoma, liposarcoma Mucus/proteinaceous material Dermoid cyst, mucocele, dacryocystocele, craniopharyngioma Melanin Melanoma Subacute blood (3 to 14 days old) Lymphangioma with blood cyst, hemorrhagic choroidal detachment, subperiosteal orbital hematoma Certain fungal infections (iron scavengers) Aspergillus a Most orbital lesions will become hyperintense after gadolinium infusion.
Excellent for diagnosing intracranial, cavernous sinus, and orbital apex lesions, many of which affect neuro-ophthalmic pathways.
Gadolinium is essential in defining lesion extent in suspected neurogenic tumors (e.g., meningioma, glioma).
All patients with clinical signs or symptoms of optic neuritis from suspected demyelinating disease should undergo brain MRI with gadolinium. Fluid-attenuated inversion recovery (FLAIR) images are especially useful. See Figure 14.3.4 and 10.14, Optic Neuritis.
For orbital studies with contrast, fat suppression (also called fat saturation) is vital to enhance the visualization of the underlying pathology (e.g., optic neuritis, fat-containing lesions). Gadolinium contrast without fat suppression may cause pathology to “disappear” into surrounding orbital fat.
Guidelines for Ordering the Study
For the vast majority of orbital studies, a head coil is indicated to provide bilateral orbital views extending to the optic chiasm.
Intravenous gadolinium is a useful adjunct for evaluating ocular, orbital, and perineural masses. In patients who have kidney failure, sepsis, or recent major surgery, the risk of developing nephrogenic systemic fibrosis (NSF) may be a contraindication. NSF is a rare but devastating complication of gadolinium that occurs weeks to months after administration. NSF is characterized by a scleroderma-like fibrosis of the skin, especially over extremities and trunk, which may involve the viscera. There is no known effective therapy or prophylaxis. Evaluate renal function in patients in whom renal insufficiency is suspected and discuss options with your radiology and nephrology departments. Gadolinium deposition of the brain has been noted in patients undergoing serial imaging. The clinical significance of this finding is unknown and is under review by the Food and Drug Administration.
Contraindications for MRI include severe claustrophobia, marked obesity, some cardiac pacemakers, some cardiac valves, suspected magnetic intraocular/intraorbital foreign bodies, spinal stimulators, vagal nerve stimulators, stapes implants, and specific breast and penile implants. Titanium plates and newer aneurysm clips are MRI safe, as are gold and platinum weights placed in the eyelids. When in doubt, ask the radiologist to look up the specific device in an MRI safety catalog. Any patient with a poorly documented implanted device should NOT be scanned with MRI until the issue is clarified. On occasion, specific types of pacemakers must be turned off and reset for an MRI.