Acute angle-closure glaucoma associated with pupillary block: The central anterior chamber depth is decreased, but more pronounced peripheral shallowing with iris bombé, giving the iris a convex appearance. See 9.4, Acute Angle Closure Attack.
Aqueous misdirection syndrome: Marked diffuse shallowing of the anterior chamber both centrally and peripherally, often after cataract extraction or glaucoma surgery. See 9.16, Aqueous Misdirection Syndrome/Malignant Glaucoma.
For other disorders, see 9.4, Acute Angle Closure Attack.
Types
Plateau iris configuration: Because of the anatomic configuration of the angle, acute angle-closure glaucoma can develop from only a mild degree of pupillary block. These angle closure attacks may be treated with a laser PI to break any component of pupillary block but this is not curative.
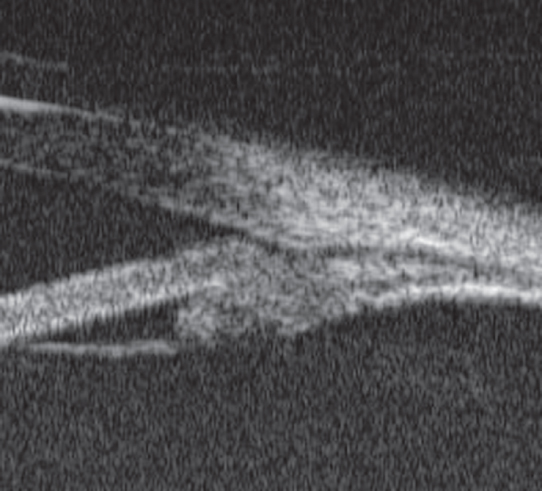
Plateau iris syndrome: The peripheral iris can bunch up in the anterior chamber angle and obstruct aqueous outflow without any element of pupillary block. The plateau iris syndrome is present when the angle closes and the IOP rises after dilation, despite a patent PI, and in the absence of phacomorphic glaucoma. UBM findings are characterized by an anteriorly rotated ciliary body. See Figure 9.12.1.