Decreased vision, often sudden; can be severe. History of compression injury to the head, chest, or lower extremities (e.g., long bone fractures). Not from a direct ocular injury.
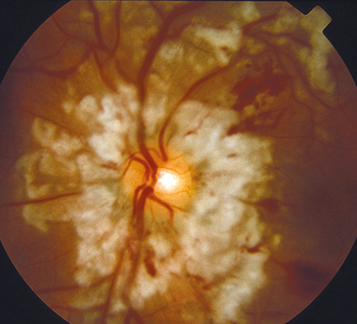
(See Figure 3.16.1.)
Multiple cotton-wool spots and/or intraretinal hemorrhages in the posterior pole; can also have polygonal areas of retinal whitening which spare the perivascular space (Purtscher flecken). Changes are typically bilateral but may be asymmetric or unilateral.
Serous macular detachment, dilated tortuous vessels, hard exudates, optic disc edema (though the disc usually appears normal), macular pseudo–cherry-red spot, RAPD, and optic atrophy when chronic.
Purtscher-like retinopathy: Several entities with the same or similar presentation but not associated with trauma (Purtscher retinopathy by definition occurs with nonocular trauma), including acute pancreatitis, malignant hypertension, preeclampsia, thrombotic thrombocytopenic purpura (TTP), hemolytic uremic syndrome (HUS), collagen vascular diseases (e.g., systemic lupus erythematosus, scleroderma, dermatomyositis, Sjögren syndrome), chronic renal failure, amniotic fluid embolism, retrobulbar anesthesia, orbital steroid injection, and alcohol use, among others.
Central retinal vein occlusion: Unilateral, multiple hemorrhages and cotton-wool spots diffusely throughout the retina. See 11.8, Central Retinal Vein Occlusion.
Central retinal artery occlusion: Unilateral retinal whitening with a cherry-red spot; see 11.6, Central Retinal Artery Occlusion.
Commotio retinae: confluent area of retinal whitening after ocular trauma. See 3.13, Commotio Retinae.
It is felt that the findings are due to occlusion of small arterioles in the peripapillary retina by different emboli depending on the associated systemic condition: complement activation, fibrin clots, platelet–leukocyte aggregates, or fat emboli.
History: Compression injury to the head or chest? Long bone fracture? If no trauma, any symptoms associated with causes of Purtscher-like retinopathy (see above, e.g., renal failure, rheumatologic disease)?
Complete ocular evaluation including dilated fundus examination. Rule out direct globe injury.
If characteristic findings occur in association with severe head or chest trauma, then the diagnosis is established and no further workup is required. Without trauma, the patient needs a systemic workup to investigate other causes (e.g., blood pressure measurement, basic metabolic panel [BMP], CBC, amylase, lipase, rheumatologic evaluation).
Fluorescein angiography: Shows patchy capillary nonperfusion in regions of retinal whitening.
No ocular treatment available. Must treat the underlying condition if possible to prevent further damage.
Repeat dilated fundus examination in 2 to 4 weeks. Retinal lesions resolve over a few weeks to months. Visual acuity may remain reduced but can return to baseline in 50% of cases.