Decreased vision; history of systemic HTN. Usually unilateral, but 10% bilateral.
(See Figures 11.19.1 and 11.19.2.)
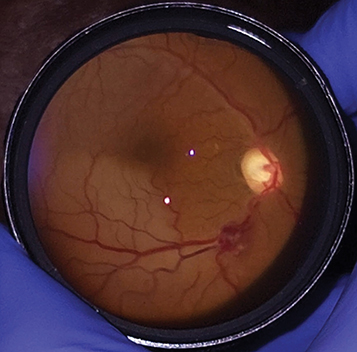
Figure 11.19.1: Retinal artery macroaneurysm on presentation.

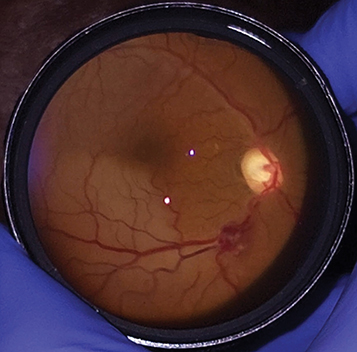
Figure 11.19.2: Intravenous fluorescein angiography of a retinal artery macroaneurysm.

Critical
Acute hemorrhages in multiple layers of the retina (subretinal, intraretinal, preretinal) possibly with VH; often with a white or yellow spot in the middle of the RAM. Chronic leakage may cause a ring of hard exudates and retinal edema around the aneurysm resulting in decreased vision if the macula is involved.
Other
ME, arteriolar emboli, capillary telangiectasia, arterial or venous occlusions distal to macroaneurysm.
Acquired vascular dilation of retinal artery or arteriole usually at the site of arteriolar bifurcation or arteriovenous crossing. Usually related to systemic HTN and general atherosclerotic disease.
Consider laser treatment if edema and/or exudate threatens central vision. Caution must be taken when treating arterioles that supply the central macula since distal thrombosis and obstruction with resultant ischemia can occur. Laser can also cause aneurysmal rupture resulting in retinal and VH. Anti-VEGF agents may be beneficial in patients with macroaneurysm-associated ME. Dense or nonclearing VH, sub–internal limiting membrane (ILM) hemorrhage, or thick submacular hemorrhage may benefit from vitrectomy (See Figure 11.19.3).
Figure 11.19.3: Retinal artery macroaneurysm with distal branch retinal artery occlusion.
Frequency based on the amount and location of exudate and hemorrhage.