Blind spot in the visual field or loss of vision, usually unilateral.
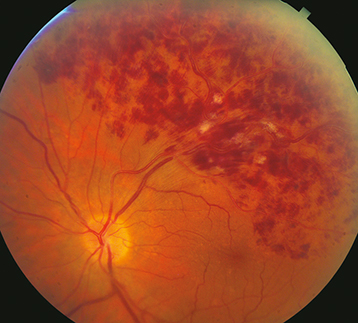
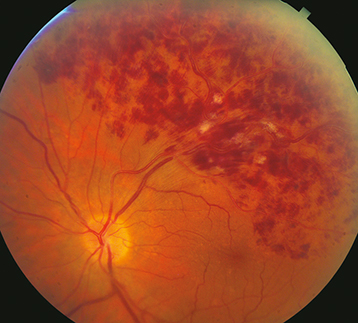
(See Figure 11.9.1.)
Figure 11.9.1: Branch retinal vein occlusion.
Critical
Superficial hemorrhages in a sector of the retina along a retinal vein. The hemorrhages usually do not cross the horizontal raphe (midline).
Other
CWSs, retinal edema, a dilated and tortuous retinal vein, narrowing and sheathing of the adjacent artery, retinal neovascularization, VH.
Disease of the adjacent arterial wall (usually secondary to HTN, arteriosclerosis, or diabetes) compresses the venous wall at a crossing point.
Retinal neovascularization: Sector PRP to the ischemic area, which corresponds to area of capillary nonperfusion on IVFA. Anti-VEGF medications can also be used particularly if there is concomitant ME.
Prompt and appropriate treatment of underlying medical conditions (e.g., HTN).
BRVO-Related Macular Edema
Anti-VEGF treatment is now the gold standard. Intravitreal ranibizumab 0.5 mg, faricimab 6 mg, and aflibercept 2 mg are FDA-approved for treating RVO-associated ME. Intravitreal bevacizumab has also been used off-label. Risks of intravitreal injection are low but include VH and endophthalmitis.
Focal retinal laser photocoagulation has historically been the standard treatment if edema is present for 3 to 6 months duration, and visual acuity is below 20/40 with macular capillary perfusion. However, anti-VEGF treatment has supplanted laser. Limitations of focal laser include length of time before effect (often several months) and the need to wait until retinal hemorrhages clear as well as less chance of visual improvement versus anti-VEGF therapy.
Dexamethasone intravitreal implant or off-label intravitreal steroid (e.g., triamcinolone 40 mg/mL, inject 1 to 4 mg). See 11.8, Central Retinal Vein Occlusion.
In general, every month initially, with gradual interval taper based on vision, presence of ME, and treatment response. At each visit, the patient should be checked for neovascularization and ME.