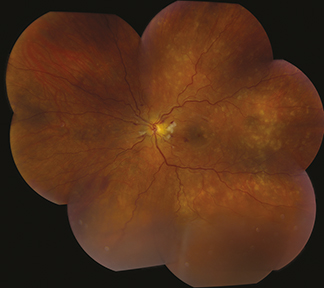
(See Figure 11.10.1.)
Figure 11.10.1: Chronic hypertensive retinopathy with arteriolar narrowing and arteriovenous nicking.
Generalized or localized retinal arteriolar narrowing, almost always bilateral.
Chronic HTN: Arteriovenous crossing changes (“AV nicking”), retinal arteriolar sclerosis (“copper” or “silver” wiring), CWSs, flame-shaped hemorrhages, arterial macroaneurysms, central or branch occlusion of an artery or vein. Rarely, neovascular complications can develop.
Acute (“malignant”) HTN or accelerated HTN: Hard exudates often in a “macular star” configuration, retinal edema, CWSs, flame-shaped hemorrhages, optic nerve head edema. Rarely serous RD or VH. Areas of focal chorioretinal atrophy (from previous choroidal infarcts [Elschnig spots]) are a sign of past episodes of acute HTN.
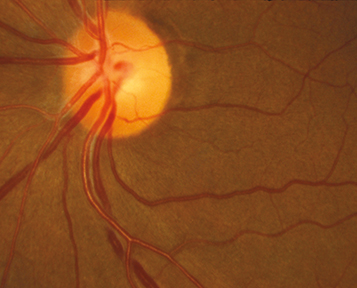
(See Figure 11.10.2.)