One of the following, almost always located at the 3-o’clock or 9-o’clock perilimbal position.
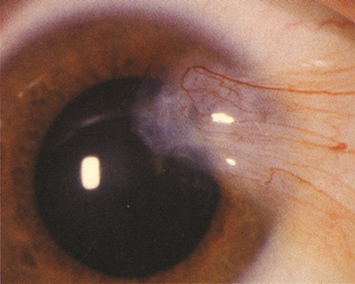
Pterygium: Wing-shaped fold of fibrovascular tissue arising from the interpalpebral conjunctiva and extending onto the cornea. There is no associated thinning of the cornea below these lesions. Usually nasal in location (see Figure 4.9.1).
Pinguecula: Yellow-white, flat, or slightly raised conjunctival lesion, usually in the interpalpebral fissure adjacent to the limbus, but not involving the cornea.
Either lesion may be highly vascularized and injected or may be associated with SPK or delle (thinning of the adjacent cornea secondary to drying). An iron line (Stocker line) may be seen in the corneal epithelium just beyond the leading edge of a pterygium, indicative of chronicity.