This chapter focuses on three critical concerns in the nursing profession: (1) nursing education, (2) quality of nursing education, and (3) regulatory issues, such as licensure. These concerns are interrelated and change, dependent on each other (for example, graduating from an accredited program is required for licensure), and require regular input from the nursing profession. Even after graduation, nurses should be aware of educational issues, such as appropriate and reasonable accreditation of nursing education programs and ensuring that regulatory issues support the critical needs of the public for quality health care and the needs of the profession. The Tri-Council for Nursing was established in 1977 and now is an alliance of five nursing organizations (American Association of Colleges of Nursing [AACN], American Nurses Association [ANA], American Organization for Nursing Leadership [AONL], National Council of State Boards of Nursing [NCSBN], and National League for Nursing [NLN]). In 2010, the Tri-Council issued a consensus policy statement following the U.S. Congress's passage of the Affordable Care Act (ACA). This demonstrates the engagement of the nursing profession in health policy and its collaborative efforts with other healthcare professionals, nursing education, and regulation. This Tri-Council policy statement included the following: “Current healthcare reform initiatives call for a nursing workforce that integrates evidence-based clinical knowledge and research with effective communication and leadership skills. These competencies require increased education at all levels. At this tipping point for the nursing profession, action is needed now to put in place strategies to build a stronger nursing workforce. Without a more educated nursing workforce, the nation's health will be further at risk” (Tri-Council for Nursing, 2010, p. 1). This statement is in line with the Institute of Medicine's (IOM, 2003) recommendations for healthcare profession education. Figure 3-1 highlights the components of the education-to-practice process integrating education, regulation, and practice.
Figure 3-1 From education to practice.
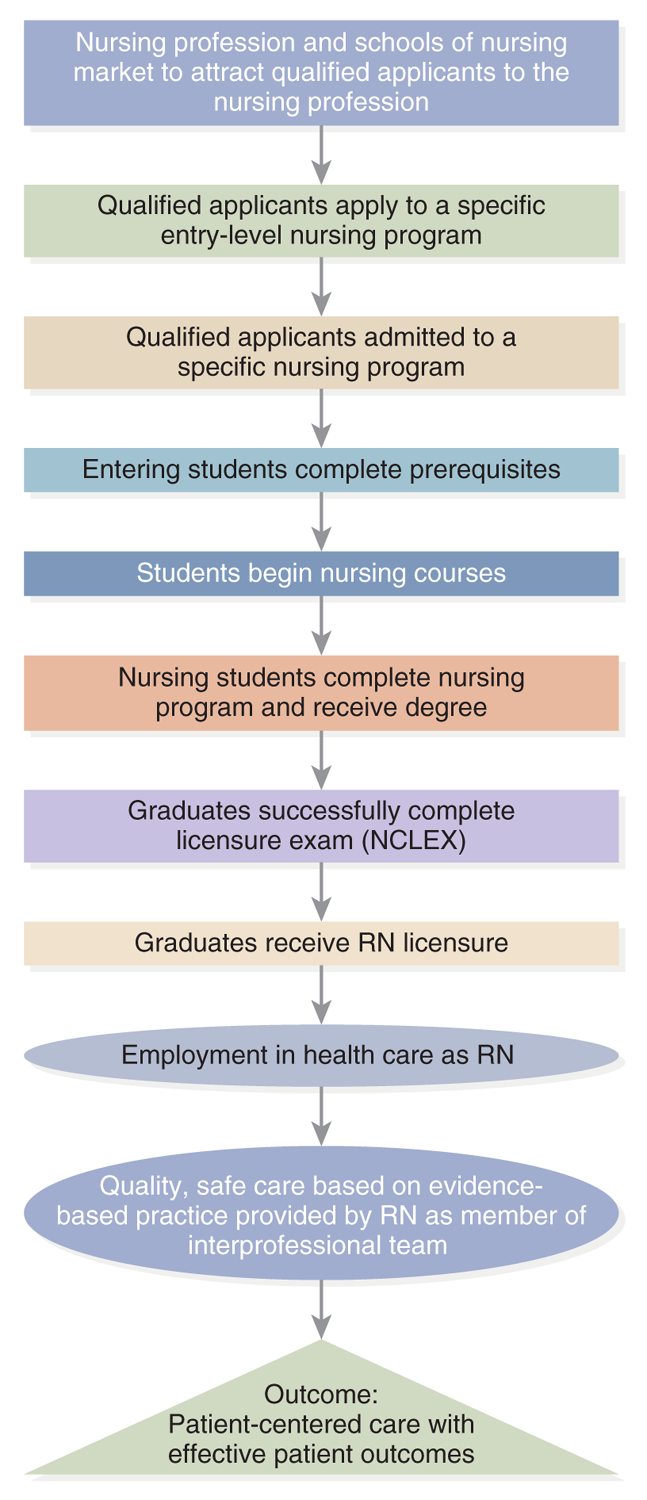
A flowchart depicts the sequential steps from initial application to employment in the nursing profession.
The flowchart depicts the process from aspiring to practicing nurse. It starts with nursing profession and schools of nursing market to attract qualified applicants to the nursing profession, followed by, qualified applicants apply to a specific entry-level nursing program. The subsequent steps are as follows: Qualified applicants admitted to a specific nursing program. Entering students complete prerequisites. Students begin nursing courses. Nursing students complete nursing program and receive degree. Graduates successfully complete licensure exam, N C L E X. Graduates receive R N licensure. Employment in health care as R N. The final step emphasizes Quality, safe care based on evidence-based practice provided by R N as a member of interprofessional team, leading to the outcome of patient-centered care with effective patient outcomes.
Nursing Education
Nursing students may wonder why a nursing text has a chapter that includes content about nursing education. By the time students are reading this text, students have selected a nursing program and enrolled. This content is not included here to help someone decide whether to enter the profession or which nursing program to attend. Rather, it is essential content because education is a critical component of the nursing profession. Nurses need to understand the structure and process of their profession's education, quality issues, and current healthcare and professional issues and trends and should, throughout their careers, be concerned with the profession's education and advocate for improvement and support of students. The following content discusses important elements that impact nursing education.
The education level of entry into practice is an important element. Data from the 2022 National Nursing Workforce Survey, reported in 2023, indicated positive news about the number of registered nurses (RNs) with a baccalaureate degree in nursing (BSN) or higher degree. The percentage of BSN nurses was 71.7% (AACN, 2023a; Smiley, 2022). The Future of Nursing report recommended that the proportion of RNs with baccalaureate degrees should be 80% by 2011; although this goal has not been met, the survey data represent improvement (IOM, 2011). There also has been an increase in Registered Nurse-Bachelor of Science in Nursing (RN-BSN) program enrollment and graduates, which is very positive, supporting the goal. These nurses did not enter nursing with a BSN but pursued it later, even though they are RNs. A critical factor in increasing the number of BSN graduates is increasing enrollment in BSN programs. Data from 2022 indicate that “for the first time since 2000, enrollment in generic baccalaureate programs declined slightly compared to the previous year. When comparing the schools that reported in both 2021 and 2022, enrollment decreased by 3,518 students (1.4%), contrasted with the 2.8% increase between 2020 and 2021. From 2021 to 2022, enrollment decreased in public colleges and private/religious colleges. Private/secular schools and colleges did not see any decline in enrollment. Non-profit institutions had a decline of 7,255 students (3.3%) while for-profit schools had an increase of 3,737 students (10.4%). The North Atlantic, Midwest, and South all experienced a decline in generic baccalaureate enrollment. The greatest declines were seen in the Midwest and North Atlantic regions of the US” (AACN, 2022a; 2023a). Qualified applicants to baccalaureate and graduate nursing programs may be rejected due to numerous factors, such as lack of faculty, clinical sites, classroom space, clinical preceptors, and budget limitations. These factors act as barriers to increasing enrollment and then graduation. These barriers need to be resolved to meet the goals of higher levels of education and completing nursing programs to achieve licensure.
The percentage of minorities enrolling in nursing programs is also an important factor for the profession and health care, and this has increased. Data indicate that there has been improvement in the number of applicants to the various nursing degree programs and in enrollment rates related to student diversity, but much work remains to reach the desired levels to meet the needs of healthcare delivery. For example, an NLN survey reported in 2022 indicated the following: “In the academic year analyzed, nearly 59 percent of students enrolled in basic RN programs are white while 14.6 percent are African American. Hispanic students make up the next largest minority group, at 13 percent, followed by Asian or Pacific Islander at 9 percent and Native Americans at 0.5 percent. By contrast, full-time faculty are racially imbalanced, with more than 76 percent identified as white, while Black nurse educators make up only 4.2 percent of faculty, Hispanics at 11 percent, Asian or Pacific Islander at 4.2 percent, and Native Americans at 0.3 percent. Demographics of sex and gender are similarly skewed. Men make up only 8.1 percent of full-time nurse educators and male nursing students make up just 13.3 percent of RN candidates. Transgender, genderqueer, or gender nonbinary individuals are three-tenths of one percent of full-time faculty and 0.1 percent of enrolled RN students are genderqueer or gender nonbinary” (NLN, 2022a). These demographics impact role models for students, who need to view the profession as diverse. Faculty and student diversity is an ongoing issue in nursing. “Nursing's leaders recognize a strong connection between a culturally diverse nursing workforce and the ability to provide quality, culturally competent patient care. Though nursing has made great strides in recruiting and graduating nurses that mirror the patient population, more must be done before adequate representation becomes a reality. The need to attract students from underrepresented groups in nursing-specifically men and individuals from African American, Hispanic, Asian, American Indian, and Alaskan native backgrounds-is a high priority for nursing profession” (AACN, 2023b). This improvement will impact access to care, health equity, and patient outcomes, but it means that nursing education must consider diversity within the school and include content about diversity, equity, and inclusion (DEI) and consider these factors during clinical experiences so that the workforce will be better prepared and understand these critical issues.
It is important to recognize that when reviewing reported data, there is a lag between data collection and analysis, and thus, not to the current year. Though many organizations, such as the American Association of Colleges of Nursing (AACN), periodically provide updated data, as does the National League for Nursing (NLN), it is not yet clear the impact that the COVID-19 pandemic might have long-term on student enrollment, completion, and so on. For example, there was a decrease in nursing enrollment in 2020, and some potential applicants were reconsidering graduate-level nursing education due to financial issues and other concerns, such as fear of exposure to COVID-19 and the use of learning technologies and remote learning (Robinson, 2021). Other nursing education issues associated with the experience of COVID-19 noted by Robinson are: Need for the nursing education to keep up with practice, such as in the area of expanding technology use, including digital health; use of different educational methods, such as online courses due to the disruption of nursing education to meet demands of COVID-19, and now greater need for more collaborative and reflective learning environments; preceptor shortage for advanced practice nursing students; difficulties meeting clinical learning experiences for students; need for improved efforts to provide ethical and civil workplaces and assist students in understanding ethical professional practice; and addressing the nursing shortage, which is a global shortage. “Multiple conclusions can be drawn. First, while challenges in nursing education may seem recalcitrant, the COVID-19 pandemic has demonstrated that rapid change is possible. The sustainability of such change is yet to be determined. Second, courageous and ingenious work is being done by leaders in nursing education to chart a bold new future that will include technological innovation, pedagogical reform, foresight thinking, and ethical reform. Finally, what remains constant is the commitment of the academic nursing community to the profession's future by focusing on students' success and well-being” (Robinson, 2021).
A Brief History of Nursing Education
It is impossible to discuss the history of nursing education without reflecting on the history of the profession and the history of health care, as discussed in other chapters-all three are interconnected.
A key historical nursing leader was Florence Nightingale. She changed not only the practice of nursing but also nurses' training, which eventually came to be called “education” rather than “training.” Training focuses on fixed habits and skills; uses repetition, authority, and coercion; and emphasizes dependency, while education focuses more on self-discipline, responsibility, accountability, and self-mastery (Donahue, 1983). Up until the time that Nightingale became involved in nursing, there was little, if any, training for the role. Apprenticeship was used to introduce new recruits to nursing, and often, it was not done effectively. As nursing changed, so did the need for more knowledge and skills, leading to increasingly structured educational experiences. This did not occur without debate and disagreement regarding the best approach. What happened as this was debated, and how does it impact nursing education today?
In 1860, Nightingale established the first school of nursing, St. Thomas, in London, England. She was able to do this because she had received a very good education in the areas of math and science, which was highly unusual for women of her era, and she acknowledged the value of formal education. With her experience in the Crimean War, Nightingale recognized that many soldiers were dying not just because of their wounds but also because of infection and a failure to place them in the best situation for healing. To improve care and apply what she learned during the war, she devoted her energies to upgrading nursing education, with less on-the-job training and more focus on a structured educational program of study, creating a nurse-training school. This training school and those that followed were associated with hospitals and became a source of cheap labor. Students were provided with some formal nursing education, but they also worked long hours in hospitals and were the largest staff source. Over time, this apprenticeship model became more structured and included a more formal educational component. This model was not ideal, although it expanded and improved. During the same era, similar programs opened in the United States. These programs eventually became known as “diploma or hospital schools of nursing.”
Hospitals across the United States began to open schools similar to those in Britain because they realized that students could be used as staff in the hospitals. The quality of these schools varied widely because there were no standards aside from what the individual hospital wanted to do. A few schools recognized early on the need for more content and improved teaching. Over time, some of these schools were creative and formed partnerships with universities so that students could receive some content through an academic institution. Despite these small efforts to improve, the schools continued to be very different from one another, and there were concerns about the lack of standardized quality nursing education.
Major Nursing Reports: Improving Nursing Education
In 1918, an important step was taken through an initiative supported by the Rockefeller Foundation to address the issue of diploma schools of nursing. This initiative culminated in the Goldmark Report (Nursing and Nursing Education in the United States), the first of several major reports about U.S. nursing education. The report included the following key points, which provide a view of some of the common concerns about nursing education in the early 1900s (Goldmark, 1923):
- Hospitals controlled the total educational hours, offering minimal content and, in some cases, no content even when that content was needed.
- Inexperienced instructors with few teaching resources often taught science, theory, and practice of nursing.
- Graduate nurses had limited experience and time to assist the students in their learning and supervise other students.
- Classroom experiences frequently occurred after the students had worked long hours, even during the night.
- Students typically were able to get only the experiences that their hospital provided, with all clinical practice experiences located in one hospital. Consequently, students might not get experiences in specialties, such as obstetrics, pediatrics, and psychiatric-mental health.
The Goldmark Report had an impact, particularly through its key recommendations to (1) separate university schools of nursing from hospitals (this represented only a minority of the schools of nursing); (2) change the control of hospital-based programs to schools of nursing; and (3) require a high school diploma for entry into any school of nursing. These recommendations represented suggestions for major improvements in nursing education. New schools opened based on the Goldmark recommendations, such as schools associated with Yale University (New Haven, Connecticut) and Case Western Reserve University (Cleveland, Ohio). It is important to recognize that at this time there was no nursing licensure.
In 1948, the Brown Report was also critical of the quality of nursing education and noted limited improvement since the Goldmark report (Brown, 1948). This led to the implementation of an accreditation program for nursing schools to be conducted by the NLN. Accreditation is a process of reviewing a school's actions and outcomes and reviewing its curriculum based on established standards. The movement toward the university setting and away from hospital-based schools of nursing and the establishment of standards with an accreditation process were major changes for the nursing profession. The ANA and the NLN continue to establish standards for practice and education and support the implementation of nursing standards, for example, the ANA Nursing Scope and Standards of Practice (2021). In addition, the AACN also developed a nursing education accreditation process, which will be discussed later in this chapter. Changes were made, but slowly. The NLN started developing and implementing standards for schools, but it took more than 20 years to accomplish this mission.
A more current report on the assessment of nursing education was published in 2010, Educating Nurses: A Call for Radical Transformation (Benner et al., 2010). This report addressed the need to better prepare nurses to practice in a rapidly changing healthcare system to ensure quality care. The conclusions from this qualitative study on nursing education were that there was a need for more improvement and offered the following recommendations. Students should be engaged in the learning process. There needs to be more connection between classroom experience and clinical experience, with a greater emphasis on practice throughout the nursing curriculum. Students should be better prepared to use clinical reasoning and judgment and understand the trajectory of illness. To meet the recommendations of this landmark report, nursing education needed to make major changes and improvements. Exhibit 3-1 describes the report's recommendations, which laid the groundwork for improvement.
| Exhibit 3-1 Recommendations from Educating Nurses: A Call for Radical Transformation |
|---|
| Entry and Pathways |
|
| Student Population |
|
| The Student Experience |
|
| Teaching |
|
| Entry to Practice |
|
| National Oversight |
|
A more recent report on the nursing profession, published by the IOM (2011), The Future of Nursing: Leading Change, Advancing Health, delineated several key messages for nurses and also nursing education. Nurses should practice to the fullest extent possible based on their level of education. There should be mechanisms for nurses to easily advance their education, act as full partners in healthcare delivery, and be involved in policy-making, especially as it relates to the healthcare workforce. This report, along with the report by Benner and colleagues (2010), led to a transformation of nursing's role in health care and changes in nursing education to support this practice transformation. In late 2015, a progress report was published to assess the current status of The Future of Nursing recommendations (National Academy of Medicine [NAM], 2015). This report is discussed further in other chapters; however, it is important to note that in this discussion about nursing education, accreditation, and regulation, many of the recommendations require more work, and some have been achieved. The report, The Future of Nursing 2020-2030: Charting a Path to Achieve Health Equity (NAM, 2021) notes the following: “The decade ahead will test the nation's nearly 4 million nurses in new and complex ways. Nurses live and work at the intersection of health, education, and communities. Nurses work in a wide array of settings and practice at a range of professional levels. They are often the first and most frequent line of contact with people of all backgrounds and experiences seeking care, and they represent the largest of the health care professions.” This comment and the report have important implications for nursing education.
Entry Into Practice: A Long Debate
The challenges in making changes in the expected education level for entry into practice debate were great when one considers that a very large number of hospitals in communities across the country had diploma schools based on the old model, and these schools were part of and funded by their communities. It was not easy to change these schools or to close them without major nursing and community debate and conflict. These schools constituted the major type of nursing education in the United States through the 1960s. Some schools still exist today, but the number of diploma schools has decreased primarily because of the critical entry into practice debate. The drive to move nursing education into college and university settings was great, but there was also some support to continue with the diploma schools of nursing.
The NLN and the American Nurses Association (ANA, 1965) made strong statements endorsing college-based nursing education as the entry point into the profession. The ANA stated that “minimum preparation for beginning technical (bedside) nursing practice at the present time should be associate degree education in nursing” (p. 107). The situation was very tense. The two largest nursing organizations at the time-one focused primarily on education (NLN) and the other more on practice (ANA)-clearly took a stand. From the 1960s through the 1980s, these organizations tried to alter accreditation, advocated for the closing of diploma programs, and lobbied all levels of government (Leighow, 1996). It was an emotional issue, and even today it continues to be a tense topic because it has not been fully resolved, although stronger statements were made in 2010 to change to a baccalaureate entry level (Benner et al., 2010; IOM, 2011). In summary, since 1965, however, there have been many changes in the educational preparation of nurses:
- The number of diploma schools has gradually decreased, but they still exist.
- The number of associate degree in nursing (ADN) programs has increased. However, there was, and continues to be, concern over the potential development of a two-level nursing system-ADN and BSN-with one viewed as technical and the other as professional. In fact, this did not happen. ADN programs continue to increase, and there has been no change in licensure for any of the nursing programs-graduates of all RN prelicensure programs continue to take the same exam and receive the same license. Many ADN programs now have options to make it easier for students to continue their education and complete BSN requirements.
- BSN programs continue to increase.
- The BSN degree is an admission requirement for graduate nursing programs.
Differentiated Nursing Practice
Another issue related to entry into practice is differentiated nursing practice, which is not a new idea as it has been discussed in nursing literature since the 1990s. It is described as a “philosophy that structures the roles and functions of nurses according to their education, experience, and competence” or “matching the varying needs of clients [patients] with the varying abilities of nursing practitioners” (AONE, 1990, as cited in Hutchins, 1994, p. 52).
How does this work in practice? Does a clinical setting distinguish among RNs who have a diploma, associate degree, BSN degree, or graduate degree? Does this affect role function and responsibilities? Does the healthcare organization (HCO) even acknowledge degrees on name badges? Most HCOs note differences when it comes to RNs with graduate degrees, but many do not necessarily note other degrees, such as the BSN. This approach does not acknowledge that there are differences in the educational programs that award each degree or diploma. The ongoing debate remains difficult to resolve because all RNs, regardless of the type and length of their basic nursing education program, take the same licensing exam. Patients and other healthcare providers rarely understand the differences or even know that differences exist. A difference in salaries due to degrees is the highest level of recognition, and this is done in some healthcare organizations.
In 1995, a joint report was published by the AACN in collaboration with the American Organization of Nurse Executives (AONE) (now known as the American Organization for Nursing Leadership [AONL]) and the National Organization for Associate Degree Nursing (NOADN) (now known as the Organization for Associate Degree Nursing [OADN]) (AACN, AONE, & AOADN, 1995). This document described the BSN and the ADN graduate roles (p. 28):
- The BSN graduate is a licensed RN who provides direct care that is based on the nursing process and focused on patients/clients with complex interactions of nursing diagnoses. Patients/clients include individuals, families, groups, populations, and communities in structured and unstructured healthcare settings. The unstructured setting is a geographical or situational environment that may not have established policies, procedures, and protocols and has the potential for variations requiring independent nursing decisions.
- The ADN graduate is a licensed RN who provides direct care that is based on the nursing process and focused on individual patients/clients who have common, well-defined nursing diagnoses. Consideration is given to the patient's/client's relationship within the family. The ADN functions in a structured healthcare setting, which is a geographical or situational environment where the policies, procedures, and protocols for the provision of health care are established. In the structured setting, there is recourse to assistance and support from the full scope of nursing expertise.
Despite increased support, such as from AONL supporting the BSN as the entry-level educational requirement, this question continues to be one of the most challenging issues in the profession and has not been clearly resolved, but it is improving (AACN, 2023l). The AACN believes that “clinicians with a Bachelor of Science in Nursing (BSN) degree are well-prepared to meet the demands placed on today's nurses. BSN nurses are prized for their skills in critical thinking, leadership, case management, and health promotion and for their ability to practice across a variety of inpatient and outpatient settings. Nurse executives, federal agencies, the military, leading nursing organizations, healthcare foundations, Magnet hospitals, and minority nurse advocacy groups all recognize the unique value that baccalaureate-prepared nurses bring to health care” (AACN, 2023b).
An example of state government interest in this topic occurred in 2017 when the governor of New York signed into state law a requirement that nurses graduating from an associate degree or diploma nursing programs in New York complete a baccalaureate degree in nursing within 10 years of initial licensure. The support for this change was given as follows: “The increasing complexity of the American healthcare system and rapidly expanding technology, the educational preparation of the registered professional nurse must be expanded” (AACN, 2019). Several studies have been conducted addressing this issue. A study by Aiken and colleagues (2003) indicated that there was a “substantial survival advantage” for patients in hospitals with a higher percentage of BSN RNs. Other studies (Estabrooks et al., 2005) supported these patient outcomes. McHugh and Lake (2010) examined how nurses rate their level of expertise as a beginner, competent, proficient, advanced, and expert and how often BSN graduates were selected as preceptors or consulted by other nurses for their clinical judgment. The survey, which was done in 1999 and then the data reused in this 2010 study, included 8,611 nurses. More highly educated nurses rated themselves as having more expertise than less educated nurses, and this correlated with how frequently they were asked to be preceptors or consulted by other nurses. The long-term impact of these types of studies on resolving entry into practice is unknown, but there is more evidence now to support the decision made in 1965, along with recommendations from major reports on nursing (Benner et al., 2010; IOM, 2010).
Aiken and colleagues (2014) continued with more research on these issues and published a study addressing nurse staffing and hospital mortality in nine European countries. This study received major recognition from HCOs and the media. The sample included discharge data for 422,730 patients in nine countries aged 50 years or older who had common surgeries. The survey included 26,516 nurses in the study hospitals. The findings indicated that increasing a nurse's workload by one patient increased the likelihood of a patient dying within 30 days of admission by 7%; in contrast, every 10% increase in the number of nurses with baccalaureate degrees was associated with a 7% decrease in the likelihood of a patient dying within 30 days of admission. These associations imply that patients receiving care in hospitals in which 60% of nurses had baccalaureate degrees and nurses cared for an average of six patients would have almost a 30% lower mortality than patients in hospitals in which only 30% of nurses had baccalaureate degrees, and nurses cared for an average of eight patients. The results indicated there was value in using BSN-prepared nurses in these hospitals, whereas reducing nursing staff may have a negative impact on patient outcomes. We need more research on this critical topic to better understand education, quality care, and improvement of practice.
The AACN also supports baccalaureate-prepared nurses as essential to quality health. Its current data indicate the following patient outcomes and care provided by BSN nurses (2023):
- 24% greater odds of surviving cardiac arrest
- 25% lower odds of mortality
- 10% lower odds of death in patients with Alzheimer's disease and related dementias
- 32% decrease in surgical mortality cases
- 8% decrease in length of stay
With increasing interest in BSN-prepared nurses since early studies and more emphasis in the profession on completion of the BSN in the last few years, many more hospitals have implemented initiatives to hire only RNs with BSN degrees and to encourage staff members without BSN degrees to return to school. Studies such as the ones mentioned here have had an impact on increasing hospital support for RNs with BSN degrees. This decision by hospitals, however, is highly dependent on the availability of RNs with a BSN degree in the local area and has also been influenced by the Magnet Recognition Program®, which supports the BSN degree as a requirement for initial practice, though it does make this a requirement to receive Magnet recognition. In recognition of the importance of education, Magnet hospitals require that nurse managers and other nurse leaders hold a baccalaureate or higher degree at the time the HCO applies for Magnet status (ANCC, 2023).
| Stop and Consider 1 |
|---|
| Does the question of the best education entry point for nurses continue to be a challenge? What do you think about this issue? |
Types of Nursing Education Programs
Nursing is a profession with a complex educational pattern: It has many different entry-level pathways to the same license to practice and many different graduate programs. The following content provides descriptions of the major nursing education programs. Because several types of entry-level nursing programs exist, this complicates the issue and raises concerns about the best way to provide education for nursing students. Graduates of all three types of prelicensure programs (diploma, associate degree, baccalaureate) must successfully complete the same NCLEX-RN licensing examination to obtain licensure.
Diploma Schools of Nursing
Diploma schools of nursing still exist, but there are less than 100 programs. Many of these programs have transitioned to other types of degree programs-for example, by forming partnerships with colleges or universities where students might take some of their courses and partnering with ADN and BSN programs. Some have closed or converted into associate degree and baccalaureate programs. These programs still interest some employers when they are short of staff and degree programs are not meeting these needs. The Association of Diploma Schools of Professional Nursing represents these schools. Diploma schools are accredited by the NLN. Graduates take the same licensing exam as graduates from all the other types of nursing programs. The nursing curriculum is similar; the graduates need the same nursing content for the licensing exam. The students, however, typically have fewer prerequisites, particularly in liberal arts and sciences, though they do have some science content. Curricula requirements may vary in these schools because some schools allow students to take some of their required courses in local colleges.
Associate Degree in Nursing
Programs awarding an associate degree in nursing (AD/ADN) began when Mildred Montag, a nurse educator, published a book on the need for a different type of nursing program-a 2-year program that would be established in community colleges (Montag, 1959). The first programs opened in 1958. At the time Montag created her proposal, the United States was experiencing a shortage of nurses. For students, ADN programs are less expensive and shorter. The percentages of ADN and BSN programs vary from state to state. There is conflict about focusing only on BSN graduates. “The NLN advocates multiple entry points while the AACN supports BSN-entry. Greater than 50% of today's new nurses begin their careers by earning a two-year associate degree in nursing through which they achieve the requisite academic and clinical foundation to pass the licensing exam to start practice” (2018).
Montag envisioned the ADN as a terminal degree, but this perception has since changed, with the degree now typically viewed as part of a career mobility path. The RN-BSN or BSN completion programs are a way for ADN graduates to complete the requirements for a BSN. There are also LPN-ADN and LPN-BSN programs to assist licensed practical nurses in expanding their career path toward meeting requirements for registered nurse licensure. Typically, in these programs, nurses work for a time and then go back to school, often on a part-time basis, to complete a BSN in a university-level program. Some prerequisite courses must be taken before these students enter most BSN programs. Examples of additional nursing courses these students may take in the RN-BSN program are health assessment, public/community health with clinical practice, leadership and management, research/evidence-based practice, and health policy. Until recently, these students rarely took additional clinical courses, as this is not the major focus of the RN-BSN programs; however, all programs accredited by the AACN must now include some clinical practice experiences or a practicum. The Commission on Collegiate Nursing Education (AACN, CCNE, 2023), an accrediting body for the AACN, defines clinical practice experiences as “planned learning activities in nursing practice that allow students to understand, perform, and refine professional competencies at the appropriate program level” (p. 1). The content typically included for the clinical experience is public/community health, focusing on what these students typically did not cover in their ADN program. Today, many of the RN-BSN programs offer courses online, and during the COVID-19 pandemic, nursing education moved many of its courses to e-learning to allow students to continue their education. There were also struggles to meet clinical practice experience requirements, which are required for some of the nursing courses and part of graduation requirements. The type of clinical experiences can vary greatly; however, not requiring clinical practice experiences in an RN-BSN program may be a problem for students who want to later complete a graduate nursing degree.
ADN and BSN programs have increased their efforts to partner with each other to provide a seamless transition from one program to the other. Establishing an articulation agreement describing partner responsibilities, benefits to the students, and how the students meet the expected BSN outcomes or competencies clarifies these partnerships (AACN, CCNE, 2019). “Articulation agreements are important mechanisms that enhance access to baccalaureate-level nursing education. These agreements support educational mobility and facilitate the seamless transfer of academic credit between associate degree (ADN) and baccalaureate (BSN) nursing programs” (AACN, 2019). Academic progression supports “lifelong learning through the attainment of academic credentials” and is an important element for all types of nursing education programs (OADN, ANA, 2015, p. 5; AACN, 2023c). Articulation agreements are used to provide options for educational mobility and facilitate the seamless transfer from one nursing degree program to another. State law may mandate these agreements, which may be partnerships between individual schools or may be part of a statewide articulation plan to facilitate a more efficient transfer of credits. Typically, in these partnerships, students spend their first 2 years in the ADN program and then complete the last 2 years of the BSN degree in the partner BSN program. In these types of programs, the participating ADN and BSN programs collaborate on the curriculum and determine how to best transition students. One benefit of this model is for the first 2 years students pay the community college fees, which are lower than university fees. Another advantage is that if there is no BSN program in a community, students have the option of staying within their own community while they pursue a nursing degree and then transitioning to a more distant BSN program or completing the BSN online.
Baccalaureate Degree in Nursing
The idea for the baccalaureate degree in nursing, an entry-level degree, was introduced in the Goldmark Report (Goldmark, 1923), although it took many years for this recommendation to have an impact on nursing education. Some of the original programs took 5 years to complete, with the first 2 years focused on liberal arts and science courses, followed by 3 years in nursing courses. Most BSN programs have changed to a 4-year model, with various configurations of liberal arts and sciences and then 2 years in nursing courses. Some schools introduce students to nursing content during the first 2 years, but typically, the amount of nursing content is limited during this period. In some colleges of nursing, students are not formally admitted to the school/college of nursing until they complete the first 2 years, although the students are in the same university. BSN programs may be accredited by the NLN or through the AACN, both of which have accrediting services. (More information about accreditation appears later in the chapter.) The licensure exam is taken after the successful completion of the BSN program. A BSN is required for admission to a nursing graduate program, and this has influenced more nurses without BSN degrees to return to school to get the degree.
The movement of many nursing schools into the university setting was not all positive. Nursing programs lost their strong connection with hospitals. Rather than establish different educational models with hospitals, the nursing education community sought to get away from the control of hospitals and move to an academic setting; however, now, nursing educators and students are often more like visitors in hospitals with little feeling of partnership and connection. This has an impact on clinical experiences, in some cases limiting effective clinical learning. During the COVID-19 pandemic, nursing education emphasized more academic-practice partnerships to cope with the many problems encountered in providing effective clinical practice for students. This experience may influence improvements in the academic-practice relationship postpandemic.
Master's Degree in Nursing
Graduate education and the evolution of the master's degree in nursing (MSN) have a long history. Early in the development of graduate-level nursing, it was called “postgraduate education,” and the typical focus areas were public health, teaching, supervision, and a few clinical specialties. The first formal graduate program was established in 1899 at Columbia University Teachers College (Donahue, 1983). The NLN supported the establishment of graduate nursing programs, and these programs developed in great numbers and, over time, developed new models. For example, some of the early programs, such as Yale School of Nursing, admitted students without a BSN who had a baccalaureate degree in another major. Today, this is very similar to the accelerated nursing programs or direct entry programs in which students with other degrees are admitted to a BSN program that is shorter, covering the same basic entry-level nursing content but with an accelerated approach. “The U.S. Bureau of Labor Statistics projects that more than 275,000 additional nurses are needed from 2020 to 2030, and that employment opportunities for nurses will grow at 9 percent, faster than all other occupations from 2016 through 2026” (BLS, 2023). To reach this number, nursing education will need to develop methods to attract students and retain them to successful completion of the nursing degree. This requires quality education to prepare nurses to practice effectively. The accelerated degree program for nonnursing graduates has been used to attract more students, and schools of nursing should continue to offer this degree at both the baccalaureate and master's degree levels to increase the number of nursing graduates (AACN, 2023d). These students are typically categorized as graduate students because of their previous baccalaureate degree, even though the degree is not in nursing. Even so, they must complete prelicensure BSN requirements, including successful completion of the licensure exam, before they can enroll in nursing graduate clinical courses, and in some cases, they are not admitted to the nursing graduate program automatically until completion of a direct entry program. They must apply to the program in the same manner as any student who wants to attend a graduate program in nursing.
Master's degrees in nursing programs have evolved since the 1950s. The typical length for a master's program is 2 years, and students may attend full time or part time. The following are examples of master's degree programs:
- Advanced practice registered nurse(APRN): This is a job title that requires a minimum of a master's degree that can be offered in any clinical area, but typical areas are adult health, pediatrics, family health, women's health, neonatal health, and psychiatric-mental health. APRN graduates take certification exams in their specialty area and must then meet specific state requirements, such as for prescriptive authority, which gives them limited ability to prescribe medications. These nurses usually work in independent roles. The American Nurses Credentialing Center (ANCC) provides national certification exams for advanced practice registered nurses in a variety of areas. APRNs treat and diagnose illnesses, advise the public on health issues, manage chronic disease, and engage in continuous education to remain ahead of technological, methodological, or other developments in the field. Historically, APRNs have completed at least a master's degree in addition to the initial nursing education and licensing required for all RNs, but this is changing. Examples of some other APRN roles include certified registered nurse anesthetist (CRNA), certified nurse-midwife (CNM), clinical nurse specialist (CNS), and certified nurse practitioner (CNP) (ANA, 2020). All these nursing positions are important in health care; for example, APRNs may serve as primary care providers and are at the forefront of providing preventive care services to the public (AACN, 2023e). See the section “Doctor of Nursing Practice” that follows regarding changes in requirements for APRNs.
- Clinical nurse specialist (CNS): This master's degree can be offered in any clinical area. Specialty exams may also be taken. These nurses usually work in hospital settings. The ANCC provides national certification for CNSs in a variety of areas, as discussed later in this chapter.
- Certified registered nurse anesthetists (CRNA): This role requires a master's degree and is not offered at all colleges of nursing; however, over time, the requirements have changed. The Council on Accreditation of Nurse Anesthesia Educational Program, as part of the American Association of Nurse Anesthetists, focuses on the accreditation and certification of these programs. This educational program has been transitioning to Doctor of Nursing Practice (DNP) degree. Currently, nurse anesthetist programs must change to DNP by 2025. Because of this potential change, students entering advanced practice programs should consider the DNP. The other option is a Doctorate of Nursing Anesthesia Practice (DNAP). Both degrees are clinical practice doctorates, not “research-based doctorates.” “The most important difference between the two degrees will be for those who have a goal of obtaining a university faculty position after completion of the degree. For some state universities the DNAP will not be recognized as a terminal degree, and thus graduates who seek faculty positions will not be eligible for tenure. Aside from this, the differences between the 2 degrees are somewhat minimal” (TheCRNA, 2017).
- Certified nurse-midwife: This master's degree focuses on midwifery-pregnancy and delivery-as well as gynecologic care of women and family planning. These programs are accredited by the American College of Nurse-Midwives.
- Clinical nurse leader (CNL): This is one of the newer master's degrees, which prepares nurses for leadership positions that have a direct impact on patient care. The CNL is a provider and a manager of care at the point of care for individuals and cohorts. The CNL serves as a nurse leader and designs, implements, and evaluates patient care by focusing on care coordination, outcomes measurement, transitions of care, interprofessional communication and team leadership, risk assessment, implementation of best practices (evidence-based practice), and quality improvement. CNLs delegate and supervise care provided by the healthcare team, including licensed nurses, technicians, and other health professionals, and advocate for patients (AACN, 2023f). Certification is available for CNLs.
- Master's degree in a functional area: This type of master's degree focuses on the functional areas of administration or education. It was more popular in the past, but with the growing need for nursing faculty, there has been a resurgence of master's programs in nursing education (AACN, 2023g). In some cases, nursing colleges offer certificate programs in nursing education. In these programs, a nurse with a nursing master's degree may take a certain number of credits that focus on nursing education, and if the nurse successfully completes the NLN certification exam, the nurse is then a certified nurse educator. This provides the nurse with additional background and experience in nursing education.
Doctor of Nursing Practice
The DNP is the newest nursing degree and is a practice-focused doctoral nursing program that prepares leaders for nursing practice, including both clinical and nonclinical care (AACN, 2023h). The latter emphasis on nonclinical care was a factor in the development of many DNP programs (Mundinger & Carter, 2019). The DNP is not a traditional PhD program, although nurses with a DNP degree are also called “doctor.” However, this does not represent the same title as someone with a PhD or a medical degree. This position has been controversial within nursing and within health care, particularly among physicians (Cronenwett et al., 2011). Over time, it has become more accepted and, as noted in this content, now required more for certain specialty graduate roles.
Some of the reasons why the DNP degree was developed relate to the process for obtaining an APRN master's degree, which requires many academic credits and clinical hours. It was recognized that students should be getting more credit for their coursework and effort. Going on to a DNP program allows them to apply some of this credit toward a doctoral degree. Three-hundred and fifty-seven DNP programs are located across the United States in all 50 states and the District of Columbia, with planning being done for 106 new programs. Since the DNP was first offered 17 years ago, 60,500 nurses have graduated with this degree. The 407 DNP programs are currently enrolling students at schools of nursing nationwide, and an additional 106 new DNP programs are in planning stages (49 postbaccalaureate and 47 postmaster's programs). (AACN, 2023h). This will continue as more master's degree programs for APRNs change to DNP programs, and there is more need for nurse leaders with scientific knowledge and expertise in quality care at all levels in HCOs-all types of HCOs. It has been recognized that the DNP prepares advanced practice nurses for leadership across complex HCOs (Bowie et al., 2019). However, there is need to consider the clinical and nonclinical aspects of the DNP degree in order to ensure that APRNs can practice effectively and also that the public is not confused by nurses with a DNP degree and those who are more clinically directed-“The nursing profession must address the potential consequences of reducing the overall number of advanced practice nurse clinicians by eliminating the clinical master's degree programs without establishing a reasonable number of clinical doctoral programs” (Mundinger & Carter, 2019, p. 61).
Research-Based Doctoral Degree in Nursing
The doctoral degree (Doctor of Philosophy-PhD; research-based doctorate) in nursing has had a complicated development history. The Doctor of Nursing Science (DNSc) was first offered in 1960, but this degree program has since transitioned to other types of doctoral programs. There were PhD programs in nursing education as early as 1924, with New York University establishing the first PhD program in nursing practice in 1953. More students need to enter these programs, and this has an impact on nursing faculty because schools of nursing want faculty with doctoral degrees. Someone with a PhD is not always required to teach but is encouraged to do so. Nurses with PhDs usually are involved in research, although a nurse at any level can be involved in research and may or may not teach. PhD study typically takes place after receiving a master's degree in nursing and includes coursework and a research-focused dissertation. This process can take 4 to 5 years to complete, depending on the completion of the dissertation. Nurses with PhDs may be called “doctor”; this is not the same as the “medical doctor” title but rather a designation or title indicating completion of academic doctoral work in the same way that an English professor with a doctorate is called “doctor.” Supporting the need for more nurses with PhDs, the Robert Wood Johnson Foundation initiated a program, the Future of Nursing Scholars, to provide funding and implement a 3-year PhD program that also provides opportunities for mentorship and networking to expedite the development of nursing scholars (Newhouse et al., 2023). Nurses who have participated in this program have found this helpful, but they also note that more information needs to be shared about the differences between the PhD and the DNP with greater clarification of the benefits of the nurse scientist role.
Some schools of nursing now offer BSN-PhD or BSN-DNP option. This means the student does not have to obtain a master's degree prior to entering the program, and the students typically enter the process as BSN students and complete with a PhD or DNP degree. The goal is to increase the number of nurses with doctoral degrees as terminal degrees by encouraging nursing students to make this career decision early.
| Stop and Consider 2 |
|---|
| We have confusion in the profession over roles, degrees, and how other healthcare providers view nursing due to these issues, both at the undergraduate and the graduate level. |
Nursing Education Associations
There are three major nursing education organizations, each with some variation in their focus. These organizations are the NLN, the AACN, and the OADN, described in the following sections.
National League for Nursing
The NLN is older than the AACN. It represents several types of registered nurse programs (diploma, ADN, BSN, master's) and vocational/practical nurse programs. Accreditation of nursing education programs is discussed in a later section of this chapter. The NLN offers educational opportunities for its members (individual membership and school of nursing membership) and addresses policies and standards related to nursing education. Its mission is to “promote excellence in nursing education to build a strong and diverse nursing workforce to advance the health of our nation and the global community” (NLN, 2022b).
American Association of Colleges of Nursing
The AACN is the national organization that represents baccalaureate and graduate programs in nursing, including doctoral programs. It began in 1969 with 121 member institutions and now has approximately 865 members (public and private schools/colleges of nursing), representing 530,000 students and 54,000 faculty (AACN, 2023i). Its activities include educational research, governmental advocacy, data collection, publishing, and initiatives to establish standards for baccalaureate and graduate degree nursing programs, including implementation of the standards. The AACN goals for 2023-2025 are as follows: The AACN is (1) the driving force for innovation and excellence in academic nursing; (2) the leading partner in advancing improvements in health, health care, and higher education; (3) a resolute leader for advancing diversity, equity, and inclusion within nursing; and (4) the authoritative source of knowledge to advance academic nursing through information curation and synthesis (AACN, 2023j; 2023k). The organization also offers accreditation for baccalaureate and master's degree nursing programs, as described in another section in this chapter.
Organization for Associate Degree Nursing
The OADN began in 1984 after Mildred Montag proposed the ADN degree in 1952. The OADN, formerly known as N-OADN, is the organization that advocates for associate degree nursing education and practice. Its major goals are to collaborate in supporting quality associate degree nursing education, recognize excellence in associate degree education, support effective faculty teaching and nursing education research, support funding for students and faculty education, provide leadership for associate degree education, and advocate for the associate degree in nursing (OADN, 2023, 2020). The organization supports the academic progression of its graduates so that they can reach their full potential. The organization does not offer accreditation services. The NLN accrediting organization, the Commission for Nursing Education Accreditation (CNEA), provides accreditation for OADN programs.
| Stop and Consider 3 |
|---|
| There are three nursing education organizations, which may be due to the confusion over the degree programs and how they relate to one another. |
Quality and Excellence in Nursing Education
There is greater emphasis today on quality health care, as discussed in this text, but also, for us to have quality care, we need to have healthcare providers who meet standards for quality performance. This requires consideration of the quality of nursing education programs.
Nursing Education Standards
Nursing education standards are developed by the major nursing professional organizations that focus on education: NLN, AACN, and OADN. The accrediting bodies of the NLN and the AACN also set nursing education standards as part of their accredited nursing education programs. State boards of nursing are involved as well. In addition, colleges and universities must meet certain standards for nonnursing accreditation at the overall college or university level. Standards guide decisions, organizational structure, process, policies and procedures, budgetary decisions, admission and student progression, evaluation/assessment (program, faculty, and student), curriculum, and other academic issues. Critical standard documents published by the AACN are The Essentials, covering baccalaureate, master's, and DNP degrees (AACN, 2021). The baccalaureate Essentials emphasize the three roles of the baccalaureate generalist nurse. These standards, which are competency-based, include student-learning outcomes expected for nursing prelicensure graduates. These standards have recently been revised, as discussed in the following content. In addition, the CNEA is also revising its standards, and updates can be found on the NLN CNEA website (NLN, 2023a).
The 2021 versions of AACN (CCNE) and NLN (CNEA) standards (baccalaureate degree, master's degree, and clinical doctorate) are the newest editions of accreditation standards (AACN, 2021; NLN, 2023a). The AACN notes: “The Essentials: Core Competencies for Professional Nursing Education is a carefully crafted document that was developed following a lengthy, inclusive, and iterative process with input from hundreds of faculty and deans as well as from multiple organizational stakeholders. The Essentials Task Force spent many months engaged in listening, discerning dialogue, and compromise to ensure quality, future-thinking standards for professional nursing education. A driving context for the Essentials Task Force was differentiating between ‘change' and ‘transformation,' which are often used interchangeably. Change fixes the past; it modifies behaviors. Transformation creates the future; it modifies values, core beliefs, and desires. The re-envisioned Essentials using a competency-based education model represents transformation, a bridge to the future of academic nursing” (AACN, 2021). The new edition includes the following key information that is required for all nursing education programs accredited by the AACN through its accrediting body, the CCNE. The new standards emphasize four spheres of care: (1) disease prevention/promotion of health and well-being, (2) chronic disease care, (3) regenerative or restorative care, and (4) hospice/palliative/supportive care (AACN, 2021). The 10 domains or nursing focus areas identified in The Essentials are (pp. 11-12):
- Knowledge of nursing practice
- Person-centered care
- Population health
- Scholarship for nursing practice
- Quality and safety
- Interprofessional partnerships
- Systems-based practice
- Information and healthcare technologies
- Professionalism
- Personal, professional, and leadership development
Concepts that are interrelated with the competencies and domains are clinical judgment, communication, compassionate care, diversity/equity/inclusion, ethics, evidence-based practice, health policy, and social determinants of health (p. 12-13). The competencies are described in the AACN Essentials website, along with further information about the domains and concepts (AACN, 2021).
NLN Excellence in Nursing Education
The NLN Hallmarks of Excellence initiative identifies hallmarks or indicators of nursing education excellence focused on students, diverse and prepared faculty, continuous quality improvement, innovative and evidence-based curriculum, evidence-based learning approaches, resources supporting goals, pedagogical scholarship, and leadership supported by the NLN Center for Excellence (NLN, 2023b, c). These indicators are applied in two of the NLN's programs that recognize nursing education excellence and include the hallmarks.
The NLN Center for Innovation in Education Excellence identifies schools of nursing that demonstrate they have achieved “a level of excellence in a specific area. Through public recognition and distinction, the program acknowledges the outstanding innovations, commitment, and sustainability of excellence these organizations convey” (NLN, 2022c). These schools commit to pursuing excellence in (1) student learning and professional development, (2) development of faculty expertise in pedagogy, and/or (3) advancing the science of nursing education. The Center of Excellence (COE) award is given to a school or college of nursing-not a program within a school-and remains in effect for 4 years. Schools may apply for continuing COE designation but must continue to meet all requirements and complete the review process. After this period, the school must be reviewed again to retain the COE recognition. This NLN initiative is a good example of efforts to improve nursing education, and it provides “creative educational simulation and curriculum integration advisory services, teaching and learning resources, and professional development opportunities” (NLN, 2022b). Two focus areas that are important to education and to current public health practice are simulation and care of vulnerable populations. In providing resources in these two areas, the NLN supports effective care and health equity.
A third example of the focus on nursing education quality is the NLN Academy of Nursing Education, which emphasizes excellence in nursing education by “recognizing and capitalizing on the wisdom of outstanding individuals in and outside the profession who have contributed to nursing education in sustained and significant ways” (NLN, 2020a). It selects nurse educator fellows who demonstrate significant contributions to nursing education in one or more areas (teaching/learning innovations, faculty development, research in nursing education, leadership in nursing education, public policy related to nursing education, or collaborative education/practice/community partnerships) and continue to provide visionary leadership in nursing education. The academy inducted its first nurse education fellows in 2007 and continues to do so annually.
The AACN and NLN nursing education accreditation bodies (CCNE and CNEA) have been very involved in assisting academic nursing programs with adaptations needed to cope with offering nursing degree education during the pandemic (AACN, 2020a; NLN, 2020b). There was major concern about the impact of offering didactic content and clinical practice experiences on faculty and student safety with recognition of the need for academic/practice partnerships during a time of public health crisis and resources to assist nursing education in meeting its goals. The organizations assisted schools and programs to meet the needs in a stressful environment; for example, the CCNE provided guidance to its accredited nurse residency programs, which have had to cope with changes related to the pandemic, and AACN and NLN provided additional faculty resources.
Focus on Competencies
In 2003, the IOM published the Health Professions Education report to address the need for education in all major health professions by describing critical common competencies. The development of this report was motivated by grave concerns about the quality of care in the United States and the need for healthcare educational programs to prepare professionals who provide quality care. “Education for health professions needs a major overhaul. Clinical education [for all healthcare professions] simply has not kept pace with or been responsive enough to shifting patient demographics and desires, changing health system expectations, evolving practice requirements and staffing arrangements, new information, a focus on improving quality, or new technologies” (IOM, 2003, p. 1). The core competencies are also emphasized in the Essentials of Baccalaureate Education; however, schools of nursing need to make changes to include the competencies and, in some cases, add new content to meet these needs.
The nursing curriculum should identify the competencies expected of students throughout the nursing program. There is greater emphasis today on implementing healthcare professions competencies, particularly the core competencies for all healthcare professions identified by the Institute of Medicine as part of its reports on quality care: (1) provide patient-centered care, (2) work in interdisciplinary/interprofessional teams, (3) employ evidence-based practice, (4) apply quality improvement, and (5) utilize informatics (IOM, 2003). This does not mean that profession-specific competencies are not relevant, such as the Quality and Safety Education for Nurses (QSEN, 2023) competencies, which should also be implemented, but the IOM competencies recognize the existence of basic competencies that all healthcare professions should demonstrate. See Table 3-1 comparing the core healthcare profession competencies and QSEN competencies.
Table 3-1 Comparing the Five Healthcare Professions Core Competencies and the QSEN Competencies for NursesHealthcare Professions Core Competencies* | QSEN Competencies for Nurses** |
|---|---|
Provide patient-centered care. | Patient-centered care: knowledge, skills, attitudes |
Work on interdisciplinary [interprofessional] teams. | Teamwork and collaboration: knowledge, skills, attitudes |
Employ evidence-based practice. | Evidence-based practice: knowledge, attitudes, skills |
Apply quality improvement. | Quality improvement: knowledge, skills, attitudes |
Utilize informatics. | Safety: knowledge, skills, attitudes |
Informatics: knowledge, skills, attitudes | |
| Data from Institute of Medicine (IOM; 2003). Health Professions Education. A Bridge to Quality. The National Academies Press; QSEN Institute (2022). Pre-licensure Competencies. https://www.qsen.org/competencies-pre-licensure-ksas |
*Institute of Medicine (IOM, 2003). Health Professions Education. A Bridge to Quality. The National Academies Press. **QSEN Institute (2022). Pre-licensure Competencies. https://www.qsen.org/competencies-pre-licensure-ksas Students need to understand the expected competencies so that they can be active participants in the learning process to reach these competencies, which are used in evaluation and to identify the level of learning or performance expected of the student. Nursing is a profession-a practice profession-so performance is a critical factor. The ANA (2018) defines competency as “an expected and measurable level of nursing performance that integrates knowledge, skills, abilities, and judgment, based on established scientific knowledge and expectations for nursing practice” (p. 86). Competencies should clearly state the expected parameters related to the behavior or performance. The curriculum should support the development of student competencies by providing prerequisite knowledge and learning opportunities to meet the competency. The goal is a competent RN who can provide quality care. Supporting this view, the reenvisioning of the AACN Essentials (2021) includes a greater focus on competency-based education (Bartels, 2019):
This approach makes the student the center of learning, and the student holds some responsibility for his or her own learning. The 2021 AACN Essentials emphasize the following: “Competency-based education is a process whereby students are held accountable to the mastery of competencies deemed critical for an area of study. Competency-based education is inherently anchored to the outputs of an educational experience versus the inputs of the educational environment and system. Students are the center of the learning experience, and performance expectations are clearly delineated along all pathways of education and practice” (AACN, 2021, p. 5; 2023l). With the revision of the identification of the health professions core competencies by the IOM and associated identification of the QSEN competencies (see Table 3-1), the revision of the AACN standards connects the emphasis on these competencies. They are reflected in the standards (QSEN Institute, 2023; Wang et al., 2022). The standard domains and concepts described in this chapter are interrelated with all these initiatives. Curriculum A nursing program's curriculum is the plan that describes the program's philosophy, levels, student terminal competencies (outcomes or what students are expected to accomplish by the end of the program), and course content and course outcomes/objectives (described in course syllabi). Also specified are the sequence of courses and a designation of course credits and learning experiences, such as didactic courses (typically offered in a lecture/classroom, seminar setting, or both venues; in some cases, in online format or hybrid, combined face-to-face and e-learning) and clinical/practicum experiences. In addition, simulation laboratory experiences are included either at the beginning of the curriculum or throughout the curriculum. The nursing curriculum informs potential students what they should expect in a nursing program and may influence a student's choice of programs, particularly at the graduate level. It helps orient new students. The curriculum is also reviewed during the accreditation process and by state boards of nursing that are charged with oversight of schools of nursing within a state. To keep current, faculty need to review the curriculum regularly in a manner that allows for easy and timely changes and includes student input. Nursing education accreditation standards also have an impact on the curriculum; for example, The Essentials (AACN, 2021) provides guidelines for nursing curricula, prelicensure, and graduate programs. Didactic or Theory Content Nursing curricula may vary as to titles of courses, course descriptions and objectives/learning outcomes, sequence, number of hours for didactic content, and clinical experiences, but there are some constants even within these differences. To ensure consistency in the practice of nursing and prepare for the licensure exam, nursing content needs to include the following broad topical areas:
Many schools offer courses focused on other topics, such as informatics and genetics, though some opt to integrate this content into several courses. Quality improvement content is often weak, even though it is now considered critical knowledge that every practicing nurse needs to have if care is to be improved and should be integrated throughout the curriculum. Nursing content may be provided in clearly defined courses that focus on one overall topical area, or it may be integrated with multiple topics. Clinical experience/practicum may be blended with related didactic content-for example, pediatric content and pediatric clinical experience-such that they are considered one course; alternatively, the clinical/practicum and didactic content may be offered as two separate courses, typically in the same semester. Faculty that teach didactic content may or may not teach in the clinical setting. Practicum or Clinical Practice Experience Practicum, or clinical practice experience, is a critical component of a nursing curriculum. These experiences must be planned, correlate with the curriculum, require intensive faculty supervision, time and effort to facilitate effective learning, and focus on active student engagement in the experiences. Extensive faculty effort and coordination with clinical sites are required for effective planning, implementing, and evaluating student clinical experiences. A critical issue today for many schools is access to clinical sites. This has led to using various methods to alleviate problems in accessing clinical experience options to ensure effective clinical experiences for students-some methods have been more successful than others. The hours for practicum or clinical experiences can be highly variable within one school and from school to school (for example, the number of hours per week and sequence of days, such as practicum on Tuesdays and Thursdays from 8 a.m. to 3 p.m.). Some schools offer 12-hour clinical sessions. This type of student schedule conflicts with the acknowledgment that 12-hour work shifts may lead to staff fatigue and an increased number of errors. Some schools offer clinical experiences in the evenings, at night, and on weekends, but these schools must ensure that there is student access to faculty and that staff are prepared to assist students. It is important for students to understand the time commitment and scheduling related to clinical experience requirements, which have a great impact on students' personal lives, time with family, and social relationships. If a student is employed while going to school, scheduling and transportation may be challenging for the student, as students will be in a variety of clinical sites throughout their nursing program experiences. In addition, clinical experiences require preparation time. The types of clinical settings are highly variable and depend on the objectives and the available sites. Typical types of settings are acute care hospitals (all clinical areas); mental health/psychiatric hospitals; pediatric hospitals; women's health (may include obstetrics) clinics; public/community health clinics and other health agencies; home healthcare agencies; hospice centers, including freestanding sites, hospital-based centers, and patient homes; schools; camps; long-term care and rehabilitation facilities; health-oriented consumer organizations, such as the American Diabetes Association; health mobile clinics; homeless shelters; doctors' offices; clinics of all types; ambulatory surgical centers; emergency centers; businesses with occupational health services; and many more. In acute care, there is typically a group (8 to 10 students) assigned to a faculty member in one clinical area for hospital experiences, and faculty are present during the experience. In other settings, particularly public/community healthcare settings, faculty visit students at the site because, typically, only a few students are at each site, with the clinical group of as many as 10 students spread out at different sites. The ratio of students to faculty in clinical settings may vary depending on individual state board of nursing requirements. The number of hours per week in clinical experiences increases each year in the program, with more hours assigned at the end of the program. COVID-19 had a major impact on educational experiences for students. For example, faculty may have had problems ensuring clinical experiences due to clinical site availability, scheduling difficulties, faculty and preceptor coverage, and the need for personal protective equipment (PPE) while in the clinical site. The experience of the pandemic required schools and clinical sites to work together to ensure effective clinical learning experiences for students, sometimes using innovative methods for scheduling, access to clinical experiences, and supervision. The National Council for State Boards of Nursing (NCSBN) examined the experience and published an extensive analysis in its journal, The Journal for Nursing Regulation. The summary comments note the following: “The COVID-19 pandemic has had a profound impact on prelicensure nursing education, leading to widespread disruptions that may have implications for nursing students' learning and engagement outcomes. Understanding how the rapid shift to online and simulation-based teaching methods has affected new graduates' clinical preparedness is critical to ensure patient safety moving forward” (Martin et al., 2023, p. S3). “RN programs around the country sought to address the nearly unparalleled challenges they confronted daily over the past 3 years. This study stands as the most comprehensive assessment of prelicensure nursing education in the United States since the onset of COVID-19. It extends knowledge by linking potential deficiencies in students' didactic and clinical education during the pandemic and their early career preparedness and clinical competence, and in doing so illuminates the possible implications for patient safety moving forward” (Martin et al., 2023, p. S46). Nursing programs may use preceptors in the clinical settings in both undergraduate and graduate programs. In entry-level programs, preceptor experiences are typically used toward the end of the program, but some schools use preceptors throughout the program for certain courses, such as in master's programs. Nursing faculty and management must collaborate to develop preceptor experiences with staff assisting. A preceptor is an experienced and competent staff member (for example, an RN staff nurse may be a preceptor for undergraduate students, APRN graduate or medical doctor for APRN students, CRNA or a certified nurse-midwife for graduate nursing students in these specialties). Preceptors should have formal training to function in this role. The preceptor serves as a role model and a resource for the nursing student and guides learning. The student is assigned to work alongside the preceptor. Faculty provide overall guidance to the preceptor regarding the nature of, and objectives for, the student's learning experiences, monitor the student's progress by meeting with the student and the preceptor, and are on call for communication with the student and preceptor as needed. The preceptor participates in evaluations of the student's progress, along with the student, but the faculty member is responsible for student evaluation. The state board of nursing may dictate how many hours may be assigned to preceptor experiences for undergraduate students. At the graduate level, the number of preceptor hours is much higher. Distance Education/E-Learning Distance education/e-learning, which is typically offered online, has become quite common in nursing education. Although not all schools offer courses in this manner, this changed due to COVID-19 as there was a greater need to continue courses, and yet in-person sessions were not possible. We do not yet know the long-term impact of this increase in alternative course methods-will schools of nursing continue to offer this option after the pandemic is resolved, or what might happen if COVID-19 resurges? Distance education occurs when the faculty and student are not in the same place, and the teaching-learning experiences may be synchronous or asynchronous, typically using technology, such as the internet (AACN, 2023m): “All nursing education programs delivered solely or in part through distance learning technologies must meet the same academic program and learning support standards and accreditation criteria as programs provided in face-to-face formats, including the following:
Distance education technologies have expanded over the past few years as technology developed. Some of the common technologies that have been used are email, audiotaped instruction, conference via internet, desktop videoconference, and internet-based programming or online format-programs designed specifically for e-learning used on computers, tablets, and smartphones. There is no doubt that these methods will continue to expand as new ones are added, and some are discarded as not effective or efficient. For example, artificial intelligence (AI) is developing and may be used in education. Additional information about AI is found in other chapters. Distance education can be configured in several ways, including the following:
Traditionally, students who participate in distance education often choose to take this type of course, if there is a choice; however, it should be noted that when schools of nursing incorporated these methods due to the pandemic, there was limited choice for many students and faculty. Academic institutions made these decisions based on need and restrictions due to COVID-19, and school administration, faculty, and students had to make changes quickly. To be successful in e-learning, students need to be responsible for their own learning, with faculty facilitating their learning. Computer competencies are critical for completing coursework and reducing student stress. Nursing programs must be clear about the hardware and software required to complete coursework. The academic institution must also provide effective and timely technology support to faculty and students. Students who are organized and able to develop and meet schedules will be better able to handle course requirements. Students are more successful if they are assertive, ask questions, and request help when they need it. Effective e-learning also requires active, engaged, competent faculty, who are responsible for developing and providing an organized course and course resources that engage the students and, ideally, faculty who want to teach using these methods. Self-directed learning is important for all nursing students because it leads to a greater ability to achieve lifelong learning as a professional. There are a variety of definitions of self-directed learning, most of which are based on Knowles's definition (1975, p. 18, as cited in O'Shea, 2003, p. 62): “a process in which individuals take the initiative, with or without the help of others, in diagnosing their learning needs, formulating learning goals, identifying human and material resources for learning, choosing and implementing appropriate learning strategies and evaluating learning outcomes.” Student-centered learning approaches should focus on effective student learning by helping students apply learning-for example, problem-based learning or team-based learning. This type of approach means that nursing faculty must also change how they teach. Faculty members assume the role of a facilitator of learning, which requires establishing a more collaborative relationship between faculty and students. Faculty work with students to develop active participation and goal setting with clear strategies to meet the goals and encourage self-assessment. The flipped classroom approach is also used, for example, with content provided online, in textbooks, and so on, with the expectation that students will come to class prepared so that they can actively participate in learning activities in the classroom rather than just listen to lectures. Compared to the traditional classroom approach, distance education typically emphasizes adult teaching and learning principles more, and approaches such as the flipped classroom also incorporate these principles. Knowles (1984) originally described principles that emphasized how learners engage with this type of educational program:
As noted in the report on nursing education (Benner et al., 2010), there is a need for greater student engagement in the classroom, which emphasizes adult principles of learning, and many of the newer methods support this recommendation. The quality of distance education is as important as the quality of traditional classroom courses. Syllabi that provide the course description, credits, objectives or learning outcomes, and other information about the course and student requirements should ensure that the same general structure and expectations are followed whether a course is taught using a traditional approach or through distance education-ensuring this is part of a school's evaluation process. Student evaluation must be integrated into a distance education course just as it is in traditional courses; however, more details are typically provided in distance education course materials, and teaching-learning practices may be different. Students and faculty also need access to timely technology support so that if they have a technology problem, they can seek help so that they can meet course requirements. The use of technology and support also need to be included in the course evaluation. Schools should ensure that students provide anonymous evaluations of the course and faculty, as required for traditional course format. Accreditation of Nursing Education Programs Education accreditation is a process used to assess if an education organization meets established standards to better ensure effective programs for students that meet practice requirements. Potential nursing students may not be as aware of the accreditation of the schools they are considering, but they should be. The focus here is on educational accreditation; in other chapters, accreditation of healthcare organizations is discussed. The accrediting organization identifies minimum standards that guide the process, and nursing schools incorporate these standards into their programs. The accrediting organization then reviews the school and its programs on a specified schedule. This is supposedly a voluntary process, but, in reality, it is not. To be effective, a school of nursing must be accredited to attract faculty and students, provide funding for educational programs and research grants, and ensure graduates' eligibility to apply for licensure and attend other nursing programs, such as graduate programs. Attending a nursing program that is not accredited can lead to complications in licensure, employment, and opportunities to pursue higher degree programs. Currently, two organizations offer nursing education accreditation services: NLN and AACN, through their respective accrediting services, the CNEA and CCNE, and as noted in this chapter, both have recently undergone a review and revision of their standards, which they do periodically. What is involved in accreditation? The process is complex and takes time. Schools of nursing must pay for the review. Schools may or may not receive initial accreditation, and when they do, programs may be required to make changes. During the period in which a school is accredited, the accrediting body may determine that the school is not in compliance with the expected standards; therefore, the school may lose accreditation, or additional reviews may be required. Accreditation is not a legal requirement, but state boards of nursing require this type of accreditation from the NLN or AACN to maintain state board of nursing accreditation. Some specialty organizations accredit specific graduate programs within a school, such as the American College of Nurse Midwifery and the American Association of Nurse Anesthetists. A school may choose which organization (CNEA or CCNE) accredits its school unless the accreditor is mandated by a state agency or law; however, schools with diploma and associate degree programs can be accredited only by the CNEA, which also accredits practical/vocational programs, baccalaureate, master's, clinical doctorate, postgraduate certificates, and distance learning programs (NLN, 2023d). The CCNE does not accredit diploma and associate degree programs. The state board of nursing in each state is involved in this requirement and in its own state accreditation process. During the accreditation process, the review team assesses schools of nursing based on the accrediting organization's standards and review the school's:
The standards are periodically reviewed and revised, which may then require nursing education programs to update according to accreditation standard changes. Both accrediting organizations and their standards support diversity in nursing education missions, curricula, students, and faculty, as well as support continuous quality improvement in education; in doing so, they have an impact on developing a caring and competent nursing workforce. After a school of nursing completes a self-study based on the accreditation standards established by the accrediting organization, the written self-study results are submitted to the accrediting organization. The next step in the accreditation process is the on-site survey at the school. Surveyors, who are faculty in other similar nursing programs, visit the school after reviewing the information the school submitted prior to the on-site visit. They observe classes and clinical experience/practicum, meet with staff at clinical sites, review documents (for example, curriculum, completed student assignments, budget, faculty organization, grants, policies, and so on), and meet with school administrative staff. If the school of nursing is part of a university, the surveyors also meet with university administrative staff. In addition, they meet with faculty, students, and alumni. They typically remain at the school for several days. Students have an obligation to participate in accreditation surveys and provide feedback. The goal is the maintenance of minimum standards to ensure an effective learning environment that supports student learning and meets the needs of the profession. Schools must undergo regular reviews after they receive initial accreditation to continue their accreditation status, typically at a designated period, but such reviews may occur at any time if changes in the school or problems arise. As mentioned earlier, more nursing programs are involved in distance education. It is important to note that distance education activities are also included in accreditation and recognize that they are a part of nursing education programs. The AACN (2023m) published a statement about the implications of accreditation on distance education, which was endorsed by 14 nursing organizations: “All nursing education programs delivered solely or in part through distance learning technologies must meet the same academic program and learning support standards and accreditation criteria as programs provided in face-to-face formats, including the following:
Mechanisms for ongoing faculty development and involvement in distance education and the use of technology in teaching-learning processes are established. Appropriate technical support for faculty and students is provided. When utilizing distance learning methods, a program provides learning opportunities that facilitate the development of student clinical competence and professional role socialization and establishes mechanisms to measure these student outcomes and ensure student access to resources required for successful attainment of all program objectives. Each accreditation and program review entity incorporates the review of distance-education programs as a component of site visitor/evaluator training” (AACN, 2023m).
Critical Nursing Education Problems Today, two critical problems found in nursing education programs are faculty shortage and the need to find effective and accessible clinical experiences for students, particularly as efforts are made to increase enrollment. These complex problems require more than one solution, and they have a great impact on the quality of nursing education, student satisfaction and outcomes, and, consequently, quality nursing care. Faculty Shortage Faculty shortage has an impact on the availability of graduates to practice because it means that fewer new nurses can enter the profession. As noted earlier in this chapter, one of the reasons that potentially qualified students cannot enroll in a nursing program is a shortage of qualified faculty. A school's faculty should reflect a balance of expert clinicians who can teach and guide students, expert researchers and grant writers who can teach and meet research obligations, and expert teachers who are pedagogical scholars. Today, schools of nursing, regardless of the type of program, are struggling to meet the demand for greater enrollment of students because of the limited number of available qualified faculty, as noted earlier in this chapter. The AACN 2022 faculty survey noted that in October of that year that “a total of 2,166 full-time faculty vacancies were identified in a survey of 909 nursing schools with baccalaureate and/or graduate programs across the country (84.4% response rate). Besides the vacancies, schools cited the need to create an additional 128 faculty positions to accommodate student demand. The data show a national nurse faculty vacancy rate of 8.8%. Most of the vacancies (84.9%) were faculty positions requiring or preferring a doctoral degree” (AACN, 2022b). Demonstrating the impact of the shortage and other factors, the AACN noted that “91,938 qualified applications from baccalaureate and graduate nursing programs in 2021 due to an insufficient number of faculty, clinical sites, classroom space, clinical preceptors, and budget constraints” (2022b). The NLN also provides data about faculty shortages. It notes in its 2021-2022 survey that the three common reasons for faculty hiring challenges are (1) inability to offer competitive salaries (45%), (2) limited qualified faculty (34%), and (3) less attractive jobs due to budget or other issues (21%) (NLN, 2021b). Data can assist schools in preparing for potential problems to better ensure nurses can meet goals and demonstrate performance that is required for quality care. Another important factor related to the faculty shortage is faculty age, which impacts retirements (AACN, 2022b). The average ages of doctorally prepared nursing faculty holding the ranks of professor, associate professor, and assistant professor were 62.5, 56.7, and 50.6 years, respectively. For master's degree-prepared, for professors, associate professors, and assistant professors, the average ages were 55.0, 54.7, and 48.6 years, respectively. The data provide a prediction of the level of retirement, indicating a need for nursing programs to prepare for retirements and replacements. In addition to potential retirements, some nursing faculty have left teaching for positions in clinical settings where the salaries are higher. Responding to and preparing for future faculty shortage problems require an increased enrollment in the number of nursing graduate programs and successful completion, but this is difficult if the major reason for limiting enrollment is the faculty shortage. Strategies to address these problems include funding to allow for greater enrollment (such as for scholarships) and solutions to increase the availability of preceptors. Recruiting new faculty also means that new faculty may have limited, if any, teaching experience and then will need mentoring from experienced faculty, which takes faculty time. In addition, consideration must be given to the number of graduates from master's and doctoral programs, which are critical sources of faculty. “Enrollment in master's programs decreased by 3.8%, which translates to 5,766 fewer students enrolled in 2021 than in 2020. In addition, enrollment in PhD nursing programs was also down. Since PhD program enrollment began to dip in 2013, enrollment in these programs have decreased by 13%, from 5,145 students in 2013 to 4,476 students in 2021 (AACN, 2022b). The COVID-19 pandemic may have an impact, too, as nurses who had planned on entering graduate programs may have personal financial concerns or other factors that changed their plans. A full appreciation of this factor requires further examination. It is also difficult to attract nurses to teaching because the pay is lower than for nursing practice; for this reason, nurses with graduate degrees often opt to stay in active practice. Attracting nurses to attend graduate school is an issue, particularly at the doctoral level. The DNP degree has attracted more nurses to these advanced degree programs, but these nurses may not be interested in teaching-and the DNP program was not intended to prepare faculty but rather to prepare practitioners. The federal government offers schools of nursing opportunities to expand nursing faculty through provisions supporting funding for education so that nurses can prepare for the faculty role, and this has improved the situation. These resources vary as funding changes. The COVID-19 pandemic also had an impact on the level of funding (AACN, 2020). The HHS, with leadership from the Biden administration, noted that nurses are an essential part of the nation's health and announced that it would provide $100 million in funding to support the expansion of the nursing workforce (HHS, 2023). This funding will be used for supporting nursing education, practice, quality, and retention-pathway to registered nursing program; train nurses to deliver primary care, mental health care, and maternal health care, critical needs in communities that could be supported by training and residency and fellowship programs for primary care nurse practitioners, clinical specialists, and certified nurse midwives; and supporting faculty loan program to address the faculty shortage, which impacts admissions and completion for all levels of nursing education programs. Access to Clinical Experiences Aside from experiencing fluctuations in the number of faculty, nursing programs struggle to provide space for clinical laboratories for simulation and to secure enough clinical sites at healthcare facilities-all of this requires a certain number of faculty to meet standards for quality education and faculty-student ratios. With the drive to increase student enrollment, securing enough clinical sites to meet course objectives is a challenge for schools of nursing. The COVID-19 pandemic made this particularly difficult when some clinical sites reduced or eliminated student experiences, but maybe we can learn from this experience as different approaches were used to ensure clinical experiences (AACN, 2020). If there are several nursing schools located in the same area, the schools in the associated area may experience competition for clinical slots. This is particularly a problem in healthcare specialties that may have fewer patient services in a location, which translates into tight demand for student clinical positions-such as in pediatrics, obstetrics, and mental health. Schools of nursing need to be more innovative and recognize that every student may not get the same clinical experiences. For example, there is increasing use of nonacute care pediatric settings. Some communities do not have pediatric hospitals and may have limited beds assigned to pediatric care in other hospitals. Other sites that might be used are pediatrician offices, pediatric clinics, schools, day-care centers, and camps. For obstetrics, possible clinical sites are birthing centers, obstetrician offices, and midwifery practices. Mental health clinical experiences may take place in clinics, homeless shelters, mental health emergency and crisis centers, and even the local mental health association or other types of community organization focused on these health needs. Recognizing difficulties in getting clinical sites has forced some schools to try different solutions, as mentioned earlier. For example, some have moved away from the traditional clinical hours offered Monday through Friday during the day. Some schools are recognizing that operating on a 9-month basis with a long summer break negatively affects the availability of clinical experiences. To accommodate the needs of all schools of nursing and the need to increase student enrollment, community-area healthcare providers often collaborate with schools to determine how all these needs can be met effectively based on the community's healthcare resources. A Response and Innovation: Laboratory Experiences and Clinical Simulation Laboratory and simulation experiences have become important teaching-learning settings for developing competencies, partly because of problems in accessing clinical experiences but also because it is now recognized they provide effective learning experiences for students without risk of harm to patients. Some nursing education programs now offer master's degree programs focused on preparing faculty for simulation education. The Agency for Healthcare Research and Quality's (AHRQ's) simulation dictionary defines healthcare simulation as: “A technique that creates a situation or environment to allow persons to experience a representation of a real healthcare event for the purpose of practice, learning, evaluation, testing, or to gain understanding of systems or human actions; the application of a simulation activity to training, assessment, research, or systems integration toward patient safety” (Lioce & Lopreiato, 2022). Simulation helps students develop confidence in their skills in a safe setting before they begin caring for real patients and can help students develop teamwork competencies. This is supported by the NCSBN study on the role and outcomes of simulation in prelicensure programs, which indicated that “up to 50 percent of traditional clinical experiences under conditions comparable to those described in the study” may be used instead of clinical experiences (NCSBN, 2020a; NLN, 2015, p. 2; Hayden et al., 2014). The simulated environment provides opportunities for teams of nursing students, or ideally, interprofessional students, to work together to respond to simulated clinical situations. Student evaluation and real-time feedback can be done in a simulated structured learning situation. These experiences should be as close to real life as possible-although they are not, of course, totally real. This does not, however, mean that these learning situations are not very helpful for student learning. Clinical training laboratories that are not as high-tech as simulation centers may be used to learn basic skills. Many schools do not have their own full simulation laboratories due to the expense of setting up and running such labs. The simulation laboratory may be established through a partnership with multiple health practice educational programs and/or hospitals to reduce the financial burden on each institution and offer simulation to a variety of students, often as an interprofessional student and/or staff experience. This then requires collaboration and sharing of space and equipment. Since a simulation laboratory is expensive to develop and maintain, students need to respect the equipment and supplies and follow procedures so that costs can be managed. Faculty supervision in the simulation laboratory may be based on a higher ratio of students to faculty than the required ratio for clinical experiences, providing more cost-effective teaching and learning. With the development of more sophisticated technology, computer simulation can also be incorporated into distance education. State boards of nursing may have requirements as to the number of simulation hours that can be substituted for clinical hours, and this is a factor that needs to be considered when using simulation-it should not be used to replace important onsite clinical experiences. The COVID-19 pandemic also had an impact on simulation experiences due to difficulty in using clinical sites, with concerns about increased risk of exposure and the need for personal protective equipment (PPE) for faculty and students, which was not always available. This experience required schools of nursing to be innovative to meet educational goals (Laerdal, 2020; Jiménez-Rodrígues et al., 2020; OADN, 2020; NLN, 2020c; Fogg et al., 2020). Some of the approaches used during the pandemic may be considered for long-term use depending on the outcomes postpandemic. In December 2020, the NCSBN initiated a research study, “National Prelicensure RN Study: Assessing the Impact of COVID-19 on Nursing Education” that included 51 nursing program sites across the United States. Its purpose was to “determine the extent to which prelicensure RN programs, either traditional Bachelor of Science in Nursing (BSN) or Associate Degree in Nursing (ADN), changed their didactic and/or clinical delivery formats due to the COVID-19 pandemic. The study prospectively and longitudinally tracked student outcomes to measure engagement, academic performance, and early career experience” (NCSBN, 2020c). The study's conclusions from the 51 schools in 27 states included feedback from 1,100 faculty and students, 4,000 course observations, and 60 focus groups (Martin et al., 2023) so that we can learn from the strategies used in educational experiences during the COVID-19 pandemic to adapt to needs and problems. These students who experienced stress and had to learn in situations that were not usual are not entering the workforce ready to practice. Nurses in practice have experienced burnout and stress impacting their work and, in some cases, retention. These new nurses need extra support and practice guidance as they may not have received the practical experiences and guidance needed. In addition, the pandemic highlighted gaps in nursing education, such as the need for more content and experience related to disaster and public health emergencies. In addition, faculty need more preparation in distance education and technology. Career preparedness and clinical competency must be evaluated and improved. Other assessments about nursing and preparation for the profession have been reported. For example, in 2020, the World Health Organization (WHO) issued a report on the state of the world's nursing. When this report is reviewed, it should be remembered that it was published as the COVID-19 pandemic was expanding, and it was based on information about global nursing issues and data collected prior to the start of the pandemic. The introduction to the report notes the following about nursing: “Nurses are critical to deliver on the promise of ‘leaving no one behind' and the global effort to achieve the Sustainable Development Goals (SDGs). They make a central contribution to national and global targets related to a range of health priorities, including universal health coverage, mental health and noncommunicable diseases, emergency preparedness and response, patient safety, and the delivery of integrated, people-centered care. No global health agenda can be realized without concerted and sustained efforts to maximize the contributions of the nursing workforce and their roles within interprofessional health teams. To do so requires policy interventions that enable them to have maximum impact and effectiveness by optimizing nurses' scope and leadership, alongside accelerated investment in their education, skills and jobs. Such investments will also contribute to the SDG targets related to education, gender, decent work and inclusive economic growth” (WHO, 2020, p. xii). This report provides considerable information about global nursing and health care, an area that requires improvement in nursing education.
Transforming Nursing Education Recent reports on healthcare delivery quality and nursing education, as described in this chapter, indicate an urgent need to institute nursing education changes. The 2010 major nursing education report identified the preparation of nurses to meet these quality demands as a critical topic, and this continues to be important (Benner et al., 2010). Thus, healthcare quality improvement relies, in part, on the improvement of nursing education, which improves nurse performance. Nursing students need to be included in the ongoing evaluation of nursing education and changes. As a student, you can help by providing course feedback and participating in curriculum committees when requested. Nursing education leaders should always review content and improve the curriculum, but they must use timely, effective methods. When accreditation surveyors come to schools of nursing, they talk to students to get their feedback, recognizing that students need to be engaged in the transformation of nursing education and have valuable feedback to share as consumers. One aspect of transforming health care related to nursing education was addressed in a recent report sponsored by the AACN focusing on academic health centers (AHCs) and nursing education (academic nursing) and practice-noting that nurses are the primary caregivers and advocates for patients (Gilliss, et al. 2021; Manatt Health Project Team, 2016). The report clarifies two key terms. An academic health center is a center of multiple health-profession schools, accredited and connected to a teaching healthcare organization, such as a hospital or health system. Academic nursing is the integration of practice, education, and research associated with baccalaureate and graduate schools of nursing-academic nursing faculty demonstrate “a commitment to inquiry, generate new knowledge for the discipline, connect practice with education, and lead scholarly pursuits that improve health and health care” (Manatt Health Project Team, 2016, p. 5). The findings from the report indicated that academic nursing was not currently positioned to be a real partner in healthcare transformation-for example, nursing had limited participation in governance and faculty leadership roles in the AHCs. This needed to change and required resources to increase this participation and collaboration. An example that was identified as a barrier is the lack of nursing faculty practice that brings in income and the overreliance on tuition for academic nursing budgets. In 2016, the AACN made the following recommendations: “embrace a new vision for academic nursing, enhance the clinical practice of academic nursing, partner in preparing the nurses of the future, partner in the implementation of accountable care, invest in nursing research programs and better integrate research into clinical practice, and implement the advocacy agenda in support of a new era for academic nursing” (p. 1). In 2020, the AACN (2020b) established a foundation to develop fundraising and grant-making to increase academic nursing. Recognizing the importance of these issues, the initiative was incorporated into the AACN's 50th anniversary celebration. Another report that addressed the need for greater collaboration and communication between nursing (or any healthcare education) and practice is Strengthening the Connection Between Health Professions Education and Practice (National Academy of Medicine [NAM], 2019). The fact that a major advisory organization, such as the NAM, would hold a workshop with experts and publish the findings on this issue indicates its importance. The discussion included content on the challenges of making data-driven decisions related to workforce and training; patient roles within health care and education with an emphasis on the patient/person-centered approach while changes occur rapidly within the healthcare system; the healthcare role in workforce development; innovations in health professional training; and supporting new healthcare educators. The discussion about these topics was aimed at the critical bottom line of strengthening connections between health profession education and practice. In the end, students should have a better appreciation of what it is like to work in the real world of health care, and this requires better collaboration and recognition that both healthcare profession education and HCOs and their staff have responsibilities to ensure students are prepared to practice in an effective and safe manner. It is important that healthcare education is aware of changes in levels of patient need, health policy and delivery, science, treatment, and technology. The healthcare workforce requires ongoing learning and updating (NAM, 2016). This focus was discussed in 2016 and included not only issues related to the United States but also global health issues and related culture and health literacy. Though unknown in 2016, 4 years later, the COVID-19 pandemic occurred and emphasized the critical need to view health care from a global perspective-healthcare needs and workforce, including education, policy, sharing of information and resources, and more. For example, at the time of the 2016 meeting and subsequent report, simulation, virtual methods, and innovation were discussed, but no one knew that soon these issues would become very important in healthcare education when student clinical experience in practice settings was reduced and in-person classroom time either reduced or eliminated. The discussion also included the growing importance of team-based care and collaborations and health profession social accountability, which must be integrated into nursing education and was important during the pandemic. The COVID-19 experience required rapid changes in nursing education, though it is not clear if the changes will be permanent or if long-term education will return to where it was prior to the pandemic (Morin, 2020). This experience impacted content, how learning was designed, and the expectations of students, faculty, and academic administration. “Those of us who are responsible for educating future nurses must continue to reinforce the essential contribution nurses make to the health of society. Given the life-threatening experiences demonstrated by caring for COVID-19 patients, students who may have considered nursing as a career may no longer entertain the possibility. Nurse faculty must assure students they will be provided an education that prepares them to be knowledgeable caregivers. To do less would be a travesty and would threaten the future supply of nurses-a supply that will continue to be sorely needed” (Morin, 2020, p. 3).
Interprofessional Healthcare Education One of the healthcare profession's core competencies is focused on interprofessional teams-an important competency for nursing education, and it has an important impact on patient care (IOM, 2003). QSEN also includes this competency (2023). Emphasis on this competency has stimulated discussion to better understand interprofessional collaborative practice. In 2009, the Interprofessional Education Collaborative (IPEC) identified key competencies to meet the needs of interprofessional teams and has published several updates since that date. Initially, the IPEC identified four topical areas or domains as values and ethics, roles and responsibilities, interprofessional communication, and teams and teamwork and later added a fifth domain as the central domain: interprofessional collaboration supported by the four competencies. The preliminary 2023 draft of these competencies continues to support collaborative practice based on the following assumptions (IPEC, 2023; 2021):
The IPEC's goals are to: “(1) serve as the thought leader for advancing interprofessional education, (2) promote, encourage, and support the academic community in advancing the IPEC efforts, and (3) inform policy makers and key influencers about the important contribution the IPEC makes to addressing healthcare needs of the nation” (IPEC, 2022). This initiative now includes many different healthcare professional organizations in its membership, expanding the original 2011 group as more stakeholders recognize interprofessional work is required. Its mission is “to ensure that new and current health professionals are proficient in the competencies essential for patient-centered, community- and population-oriented, interprofessional, collaborative practice” (IPEC, 2022). These efforts strongly support the need for “safe, high-quality, accessible, patient/person-centered care for all and interprofessional collaboration is required to accomplish this” (IPEC, 2016, p. 4). Not only are healthcare profession educational programs including more on interprofessional content and experiences with interprofessional teams but there also is more faculty development on the topic. This emphasis on interprofessional teams is now included in the accreditation of educational programs. Interprofessional education occurs “when students from two or more professions learn about, from and with each other to enable effective collaboration and improve health outcomes” (WHO, 2010). To meet these needs, nursing education must work to provide effective learning experiences for nursing students so that they are prepared to work on interprofessional teams. Nursing students, prelicensure and graduate levels, also have responsibilities, such as actively engaging in the learning activities planned by faculty and seeking out learning situations that support interprofessional competencies. Students might do this by observing work teams in clinical settings, asking to join an interprofessional activity in clinical settings, and working to increase communication with and respect for other healthcare professionals and other students. COVID-19 has led to a greater need to develop different approaches to teaching and learning that might not include physical patient contact, and this also applies to interprofessional education. New approaches have been developed and are accessible on the internet, for example, iCollaborate, which can be applied to nursing education (AAMC, 2023).
Regulation In the nursing profession's early history and under the influence of Florence Nightingale, the profession had some structure and rules, which over time developed and became more important. “As a regulated profession, nursing is governed by a set of laws and rules that outline the core tenets of nursing practice, which include (a) profession entry requirements; (b) how nurses are authorized to practice; (c) what nurses are allowed to do; (d) whether continuing competence must be demonstrated and with what frequency; (e) which actions warrant discipline and the nature of that discipline; and (f) any other requirements deemed necessary to protect the public” (NCSBN, 2020b, p. 5). How are professional regulation and nursing regulation for practice licensure related? Regulation for practice or licensure is clear, though problematic in some cases. This type of regulation is based on state laws and regulations that determine licensure; however, this is different from professional regulation in which the profession itself regulates its practice. State boards of nursing are not nursing professional organizations but rather state government agencies. This distinction can make it difficult to make changes in a state's practice of nursing, which requires state legislative changes and may vary from state to state. Professional organizations have an impact on practice through the standards they propose and other elements of support and on data that they provide to guide states as they regulate practice. Licensure based on an exam began in 1950. Nursing was the first healthcare profession to require an exam for licensure, which was the State Board Test Pool, now known as NCLEX (Lundy & Masters, 2021). The major purpose of regulation is to protect the public, and it is based on the Tenth Amendment of the U.S. Constitution, the states' rights amendment. Each state has the right to regulate professional practice, such as nursing practice, within its own state, for example, by requiring an exam for licensure. The use of a national exam also supported more mobility of nurses; although nurses must still apply for a license in the states in which they practice, the exam results apply across states. In general, the regulatory approach selected should be sufficient to ensure public protection. The following are important elements in professional licensure (NCSBN, 2022, 2021, 2020b):
Today, influenced by the items mentioned previously, in summary the following eight guiding principles continue to be relevant in nursing regulation: (1) protection of the public, (2) competence of all practitioners regulated by the board of nursing, (3) due process and ethical decision-making, (4) shared accountability, (5) strategic collaboration, (6) evidence-based regulation, (7) response to the marketplace and healthcare environment, and (8) globalization of nursing (NCSBN, 2022). Nurse Practice Acts Each state has a nurse practice act that determines the nature of nursing practice within the state. The nurse practice act is a state law passed by the state legislative body. Nurse practice acts for each state can be found on state government websites. Every licensed nurse should be knowledgeable about the nurse practice act that governs practice in the state where the nurse practices under his or her RN license, and nursing students should be aware of the nurse practice act in the state in which they are enrolled as a student. Typically, nurse practice acts do the following for their state (Masters, 2021, p. 166):
The most important function of the nurse practice act is to define the scope and boundaries of practice for nurses in the state to protect public safety. State Boards of Nursing State boards of nursing implement the state's nurse practice act and recommend state regulations and changes to this act when appropriate. The board is part of state government, although how it fits into a state's governmental organization varies from state to state. RNs serve on state boards of nursing, and the governor typically selects board members who serve for a specific term of office. Licensed vocational/practical nurses (LVN/LPNs) and laypersons or consumers (nonnurses) may also have representation on the board. The primary purpose of the state board of nursing is to protect the health and safety of the public (citizens of the state). A board of nursing has an executive director who manages the business of the board, along with staff who work for the state board-all are state employees. The size of the state has an impact on the size of the board of nursing and its staff. Boards are not only involved in setting standards and licensure of nurses (RNs and LVN/LPNs) but are also responsible for monitoring nursing education (RN and LPN) programs in the state. The board serves a regulatory function; as part of this function, it can issue administrative rules or regulations consistent with state law to facilitate the enforcement of the nurse practice act to ensure the public's safety and maintain nursing performance competence. The board of nursing in each state also reviews problems with individual licensure and is the agency that administers disciplinary actions. If a nurse fails to meet certain standards, participates in unacceptable practice, or has problems that interfere with safe practice, and if any of these violations are reported to the board, the board can investigate and review the situation and determine actions that might need to be taken. Examples of these issues are assault or causing harm to a patient; having a problem with illegal drugs or with alcohol (substance use); conviction of, or pleading guilty to, a felony (examples of felonies are murder, robbery, rape, and sexual battery); and having a psychiatric illness that is not managed effectively and interferes with safe functioning. A nurse may be reprimanded by the board or denied a license, subject to suspended or revoked licensure, or face licensure restriction with stipulations (for example, the nurse must attend an alcohol treatment program to retain licensure). The board must follow strict legal procedures when taking any disciplinary action, which must first begin with an official complaint to the board. Anyone can make a complaint to the board-another nurse, another healthcare professional, a healthcare organization, or a consumer. The state's nurse practice act identifies the possible reasons for disciplinary action. Boards of nursing publish their disciplinary action decisions because they are part of the state's public record. When nurses obtain licenses in other states, they are asked to report any disciplinary actions that have been taken by another state's board of nursing. Not reporting disciplinary board actions has serious consequences for obtaining (and losing) licensure. A key point is that licensure is a privilege, not a legal right. It is important to consider this point as a student because the same rules apply when getting the first license-even if a student graduates from a nursing program, this does not mean the graduate has a right to take the NCLEX exam or to be given a license. National Council of State Boards of Nursing The NCSBN is a not-for-profit organization that represents all the boards of nursing in the 50 states, the District of Columbia, and four U.S. territories (American Samoa, Guam, Northern Mariana Islands, and Virgin Islands). Through this organization, all state boards of nursing work together on issues related to the regulation of nursing practice that affect public health, safety, and welfare, including the development of registered nurse licensing examinations-more than 6 million candidates have taken NCLEX since April 1994 (NCSBN, 2023a, b). Nursing regulation covers more than 5 million active nurses in the United States. Although the NCSBN cannot dictate change to individual state boards of nursing, it can make recommendations, which often carry significant weight. Individual state boards of nursing, unlike the NCSBN, are part of, and report to, the state government. The NCSBN strategic plan for 2023-2025 focuses on the following goals (NCSBN, 2023c):
Promote agile regulatory systems for relevance and responsiveness to change.
Champion regulatory solutions to address borderless healthcare delivery.
Strengthen the capacity, capability, diversity, and engagement of regulatory leadership.
Pioneer competency assessments to support the future of health care and the advancement of regulatory excellence. The NCSBN also provided resources and guidance to state boards of nursing and nursing education programs during the COVID-19 pandemic. Examples of these initiatives can be found on the NCSBN website. The board, in collaboration with other nursing organizations, also issued a statement supporting the use of a practice/academic partnership model during the COVID-19 crisis (2020d). This model was not mandated but was recommended to meet education and practice or workforce needs. Student and faculty participation had to be voluntary and include consideration of student and faculty safety. This model focuses on partnerships between healthcare organizations and nursing education programs so that prelicensure nursing students from all types of degree programs can be used to assist care delivery during a time of crisis and shortage, such as the COVID-19 pandemic. With this partnership, nursing students would be employed as full- or part-time staff and work in a student-nurse role supported by their school of nursing and receive academic credit for clinical work while fully enrolled in a nursing program. Some nursing education programs and HCOs initiated this model (Alexander, 2020). Licensure Requirements Each state's board of nursing determines its state's licensure requirements based on state law; however, all states require passage of the NCLEX-RN, which is a national exam. Other requirements include criminal background checks for initial licensure and continuing education (CE) for renewal, though the latter requirement varies from state to state. Many nurses hold licenses in several states, obtained through endorsement, or may be held as inactive status in some states. An RN should always maintain one license, even if not practicing, to make it easier to return to practice. Fees are paid for the initial license and for license renewal. States in which a nurse is licensed notify the nurse when the license requires renewal. It is the nurse's responsibility to complete the required forms, meet and report on any requirements, and submit payment. States offer electronic processes for these activities. Examples of initial licensure and renewal requirements, which vary from state to state, include the following:
Ultimately, each RN is responsible for maintaining competency for safe practice. Any person who practices nursing without a valid license commits a minor misdemeanor. If licensed in one state, the nurse can typically do the following in another state in which the nurse is not licensed: consult, teach as a guest lecturer, and conduct evaluations of care as part of an accreditation process. National Council Licensure Examination The NCLEX is the national nursing exam that is developed and administered through the NCSBN (2023d). There are two forms of the exam: NCLEX-RN for RN licensure and NCLEX-PN for practical nurse licensure. In each jurisdiction (state) in the United States and its territories, licensing authorities regulate entry into the practice of nursing. To ensure public protection, each jurisdiction requires a candidate for licensure to pass the examination that measures competencies needed to perform safely and effectively as a newly licensed, entry-level RN (or LPN/LVN). RN content relates to the following patient/client needs categories: safe, effective care environment (management of care, safety, and infection control), health promotion and maintenance, psychosocial integrity and diversity/equity/inclusion, and physiological integrity (basic care and comfort, pharmacologic and parenteral therapies, reduction of risk potential, physiological adaptation). The examination is offered online. Most of the questions are written at the cognitive level of application or higher, requiring the candidate to use problem-solving skills to select the best answer. The exam is a computer-adaptive test. In this type of exam, the computer adjusts questions to the individual candidate so that the exam is then highly individualized, offering challenging questions that are neither too easy nor too difficult. NCSBN provides detailed information on the exam that is important for students to review. The exam includes a variety of questions, such as multiple-response, fill-in-the-blanks, and hot spot items using a picture or graphic. The NCLEX exam has recently undergone a review and major revision that impacts its overall approach and is based on standards. The Next Generation NCLEX (NGN) change is the most significant change the exam has undergone in 30 years and was implemented in the spring of 2023. It now includes next-generation features, using real-world case studies to measure a nurse's ability to think more critically and make the right decisions. It is recognized that clinical judgment is critical to nursing practice and profession and must be addressed in entry-level practice. Clinical judgment is the process by which nurses come to understand the problems, issues, and concerns of patients, attend to salient information, and respond to patient problems in concerned and involved ways. The NGN includes both conscious decision-making and intuitive response and evaluates clinical judgment and decision-making abilities by using evolving case scenarios to measure each aspect of the NCSBN Clinical Judgment Measurement Model (NCJMM) (NCSBN, 2023e). The NCSBN provides information for student preparation for the NCLEX, including the NGN. Schools of nursing and students are involved in the NCLEX process. Students are asked by their school to complete an application for NCLEX in the final semester before graduation. This application is sent to the state board of nursing in the state where the student is seeking licensure, which may not be the state in which the student has attended the nursing program. After a student completes the nursing program, the school must verify that the student has graduated. At this point, the student becomes an official NCLEX candidate. The student receives an authorization to test, instructions, and information about scheduling the exam. The authorization to test is the nursing graduate's pass to take the exam, so it is important to keep it. Students then schedule their own exam within the given time frame. The NCSBN website provides information about the process. Testing sites are available in every state, and a candidate may take the exam in any state. Licensure, however, is awarded by the state in which the candidate has applied for licensure. On the scheduled date, the student goes to the designated testing site to take the national computerized exam. Biometrics are taken from candidates prior to taking the exam: a signature, palm vein scan, and photograph to ensure exam security and a brief orientation is also provided prior to taking the exam at the testing site. An exam session lasts several hours, but because of the computerized adaptive test method, the amount of time that an individual candidate needs for the exam varies. The amount of time is not an indicator of passing or failing. Passing scores are the same for every state and are set by the NCSBN; they can vary from year to year. Candidates are usually informed of their results within several weeks; the result is shared as “pass” or “fail,” with no specific score provided. If a candidate does not pass the NCLEX, the candidate may retake the exam based on the time schedule set by each state. Most schools of nursing provide some type of preparation (for example, throughout the nursing program or near the end); some may recommend that students complete a prep course on their own. These prep courses require a fee and are of varying length. Many publications, as well as internet resources, are also available to assist with NCLEX preparation. In reality, student exam preparation takes place every day in nursing programs-in courses and clinical experiences as students learn and practice receiving faculty feedback. Schools of nursing receive composites of student results. Data on individual school pass rates (not individual student pass rates) are available on state board of nursing websites and are open to the public. Results from the NCLEX are an important element in a school of nursing's evaluation/assessment process. A nursing program's student first-time pass rate is reviewed routinely and must be reported to the school's accreditation organization; in addition, the state board monitors these results. Schools of nursing can be put on probation by their state boards of nursing if pass rates are a problem. This leads to further evaluation of the program and monitoring of outcomes. The state boards of nursing protect students and potential students by ensuring that the education provided will prepare them at the level expected for practice. Critical Current and Future Regulation Issues Nursing regulation covers many issues related to legal requirements for nursing practice. State boards of nursing and their respective legislative bodies are responsible for nursing regulation. The NCSBN offers advice to state boards of nursing, and nursing professional organizations also offer their advice but cannot formally regulate practice. There have been some regulatory efforts at the federal level, though this is not common, but if done more routinely, it would lead to more consistent regulation across states. Nurse Licensure Compact There has been a growing need to design licensure methods that address the following situations: a nurse lives in one state but works in an adjacent state, a nurse works for a healthcare company/organization with sites in several states, and a nurse works in digital health with care provided via technology in more than one state. To address these types of issues, the NCSBN created a new model for license portability called “mutual recognition” or nurse licensure compact (NLC) (NCSBN, 2023f). Each state in a mutual recognition compact must enact legislation or regulation authorizing the use of the NLC and adopt administrative rules and regulations to implement the compact. Each compact state must also appoint an NLC administrator to facilitate the exchange of information between the states that relate to the NLC and related regulations. More than 40 states have adopted this model (NCSBN, 2023f). Some states have decided that this model is unconstitutional because it delegates authority for licensure decisions to other states. A list of current states offering this multistate licensure is available from the NCSBN website. There have been suggestions that what is needed is national licensure, but this has not yet happened. In addition to the NLC for RNs, in 2020, the NCSBN adopted the APRN Compact (NCSBN, 2023g). This change, when finally approved, will allow APRNs to practice in multiple states in the compact. The APRN compact offers states the mechanism for mutually recognizing APRN licenses and authority to practice. This will be enacted when at least seven states approve legislation supporting the APRN Compact. The COVID-19 pandemic brought digital health and interstate compact licensure issues to the forefront. Digital health is discussed later in the text, but it is important to recognize that it is connected to licensure issues. In addition to the greater use of digital health with providers interacting with patients in many states different from the provider's state of licensure or even physical location, the pandemic has required greater efficient movement of licensed healthcare providers from state to state as rates of illness changed-but how do these providers get licensed quickly in states when requested to help in another state in an emergency? In the summer of 2020, Congress introduced legislation to address this issue, such as the Equal Access to Care Act (S. 3993), to provide more flexibility in allowing healthcare providers licensed in one state to provide care in another state where the provider is not licensed, which was a problem in many states. This bill did not pass (GovTrack, 2020a). The second legislation related to a similar issue was the Temporary Reciprocity to Ensure Access to Treatment (TREAT) Act (S. 4421), allowing staff licensed in one state to obtain temporary licensure if there is a public health emergency as declared by the Secretary of HHS-this applies to digital health and practice in person. COVID-19 was this type of emergency, and this led to this proposal to temporarily allow greater levels of medical licensing reciprocity (GovTrack, 2020b). This bill did not pass. We are left with this problem, which should be addressed even when there is no public health crisis, but when we experience other crises, this will be a problem again. Digital health may, over time, impact changes to address the problem. Mandatory Overtime A critical concern in practice today is requiring nurses to work overtime. Employers make this decision, and it is called “mandatory overtime.” This policy impacts the quality of care and affects staff satisfaction and burnout. Some state boards of nursing are involved in state legislative efforts related to mandatory overtime. Although legislative and regulatory responses have provided nurses with additional support for creating safer work environments, each of these legislative responses has a significant effect on the numbers and types of nursing personnel that will be required for care delivery systems in the future, as well as on the cost of care. Clearly, there was and continues to be concern at the state and national levels by HCOs, nursing education, and nursing professional organizations about the impact of fewer staff on the healthcare quality and safety. Students and newly licensed nurses should be concerned about this issue, and during job interviews, they should ask about mandatory overtime if they are not in a state that has a law to protect them from it. Research has been done regarding sleep deprivation and its connection to the rising number of medical errors (Stimpfeil et al., 2020). This research needs to continue to provide concrete evidence linking the factors of sleep deprivation and long work hours with healthcare errors. Other work areas and professions have examined this problem and taken steps to reduce hours; for example, the aviation industry reduced the number of hours that flight crews can work without a break for sleep, and the number of hours that medical residents can work consecutively was decreased because of concern about fatigue and errors. Foreign Nursing Graduates: Entrance to Practice in the United States The number of nurses from other countries coming to the United States to work and/or study has increased. Some nurses want to work here only temporarily; others want to stay permanently. This international movement of nurses typically increases during a shortage, and today, there is a worldwide shortage and a lot of nursing migration (International Centre on Nurse Migration, 2023). This shortage had a negative impact on the care needed during the COVID-19 pandemic. An example of the stress caused by this situation is that, in early 2021, the Philippines offered Britain and Germany nurses in exchange for vaccines for the Philippines. The proposal was declined and had negative ethical and legal implications. The nurses in these countries were very upset about this proposal-they felt they were treated as commodities (CNN, 2021). Nurse migration is a complex area-affecting the country of origin, which may then experience a shortage, and there is the need to effectively integrate foreign nurses in the United States who may not have had the type of nursing education or clinical practice we expect (Jacobson, 2015). The International Centre for Nurse Migration provides resources for nurses who are moving from one country to another and information about this critical topic to increase the profession's understanding of this issue. As discussed, the NCSBN notes that each state board of nursing is responsible for RN licensure for its state. What requirements do nursing graduates of non-U.S. schools of nursing have to meet to practice in the United States? States may vary in requirements, but all internationally educated nurses must pass the NCLEX exam; comply with standards of approved or comparable education; hold a verified, valid, and unencumbered state license; and be proficient in their written and spoken English language skills (NCSBN, 2023h). The Commission on Graduates of Foreign Nursing Schools (CGFNS) International (2024) is an organization that assists these nurses in evaluating their credentials and verifying their education, registration, and licensure. This is an internationally recognized, immigration-neutral, nonprofit organization that protects the public by ensuring that these nurses are eligible and qualified to meet U.S. licensure and immigration requirements. These nurses must also take the English as a Foreign Language Exam to ensure that their English language ability is at an acceptable level. This requirement also applies to students from other countries who want to enter U.S. prelicensure or a graduate nursing education program. If a nurse from another country wants to enter a graduate nursing program in the United States, the nurse needs to get a U.S. RN license to participate in required clinical work in the educational program. Licensure must be from the state in which the nurse will meet the required clinical practice experiences. Licensure is not required to enter a prelicensure program (BSN) in nursing. Global Health Regulatory Issues With the development of the internet and digital health along with global migration, nursing has had to confront the need to examine changes related to interstate nursing practice and possible responses. Globalization has had a similar impact on migration (Fernandez & Hebert, 2004). This migration phenomenon supports the need for international credentialing of immigrant nurses to ensure public safety, but this does not yet exist. The International Council of Nurses notes that “[n]ew models for practice will continue to emerge to manage change, care, and plan for the future. Electronic technologies provide an opportunity to develop a new identity for nursing practice. New regulatory requirements will emerge to meet the needs of practitioners to ensure public safety. As a new paradigm for ensuring competencies and self-regulation in a global market evolves, the need to explore global licensure will emerge. The future belongs to those who will accept the challenge to make a difference in a global marketplace and take the necessary risks to make things happen” (Fernandez & Hebert, 2004, p. 132). The Global Alliance for Leadership in Nursing Education (GANES, 2023) is a nursing organization that focuses on encouraging nurse educators from around the world to work together to develop and facilitate nursing education and professional development for nurses worldwide to improve health care globally. These efforts recognize the need for international standards in nursing education and resolution of global nursing issues. Nursing has moved from a focus on individual hospitals to the state level, to the national level, and now to a global level.
|