Population: Hospitalized patients not undergoing surgery.
Organizations
 ASH 2018, ACCP 2016, ACP 2011
ASH 2018, ACCP 2016, ACP 2011
Prevention Recommendations
–In acutely ill patients (hospitalized, not in ICU/CCU), determine risk for VTE using Padua Prediction Score or IMPROVE score (Table 2–6). (ASH)
–Consider determining risk of bleeding using IMPROVE bleeding score or risk factors (Tables 2–7 and 2–8). (ASH)
–Do not use pharmacologic prophylaxis or mechanical prophylaxis in low-risk patients.
–Use thromboprophylaxis with LMWH in acutely ill hospitalized patients at elevated risk: equivalent of enoxaparin 40 mg SQ daily; fondaparinux 2.5 mg SQ daily. Only use low-dose unfractionated heparin (UFH) 5000 units BID or TID in patients with significant renal disease. UFH has a 10-fold increased risk of heparin-induced thrombocytopenia (HIT). Women are 2.5 times likely to develop HIT compared to men. Continue for duration of hospital stay.
–If not using pharmacological prophylaxis because of bleeding risk, use mechanical (use intermittent pneumatic compression [IPC] or graduated compression stockings [GCS]).
–If unable to use pharmacologic or mechanical prophylaxis, consider aspirin.
–Do not use both pharmacological and mechanical prophylaxis together.
–Do not use DOACs for prophylaxis unless on DOAC for some other reason.
–Do not use VTE prophylaxis in chronically ill (including nursing home), outpatients with minor risk factors, or low-risk long-distance travelers (≥4 h).
–For high-risk long-distance travelers (Table 2–9): use graduated compression stockings or LMWH.
Practice Pearls
• Routine ultrasound screening for DVT is not recommended in any group.
• 150–200,000 deaths from VTE in the United States per year. Hospitalized patients have a VTE risk which is 130-fold greater than that of community residents. (Mayo Clin Proc. 2001;76:1102)
• Neither heparin nor warfarin is recommended prophylactically for patients with central venous catheters.
• In higher risk long-distance travelers, frequent ambulation, calf muscle exercises, aisle seat, and below-the-knee graduated compression stockings (GCS) are recommended over aspirin or anticoagulants.
• Treat hospitalized inpatients with solid tumors without additional risk factors for VTE (history of DVT, thrombophilic drugs, immobilization) with prophylactic dose LMWH.
• Be cautious in patients with Ccr <20–30 mL/min—UFH or dalteparin (half-dose) preferred.
• Consider adjusted LMWH dose in patients <50 kg or ≥110 kg in weight. Monitor with heparin anti-10a activity testing.
• Inferior vena cava (IVC) filter indicated in patients with diagnosed DVT with or without pulmonary embolism (PE) who cannot be anticoagulated because of bleeding. There are no other situations where a filter has been proven to be beneficial. Do not use IVC filter prophylactically.
• Although several studies have shown survival benefit for VTE prophylaxis in surgical patients, this has not been proven in medical patients. (N Engl J Med. 2007;356:1438; 2011;365:2463)
TABLE 2–6 RISK FACTORS FOR VTE IN HOSPITALIZED MEDICAL PATIENTS
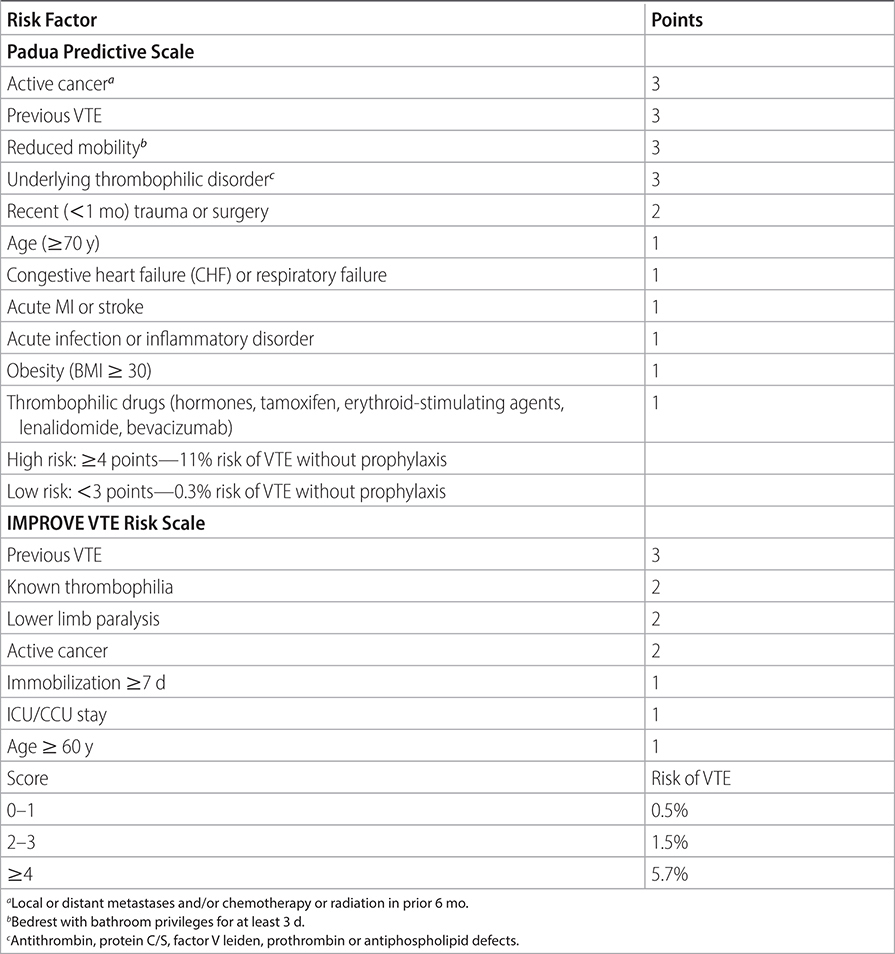
TABLE 2–7 RISK FACTORS FOR BLEEDING (CHEST. 2011;139:69–79)
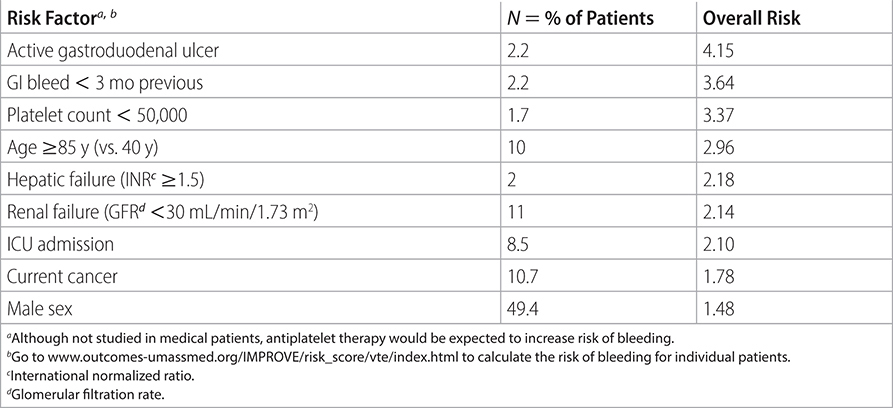
TABLE 2–8 IMPROVE BLEEDING RISK SCALE
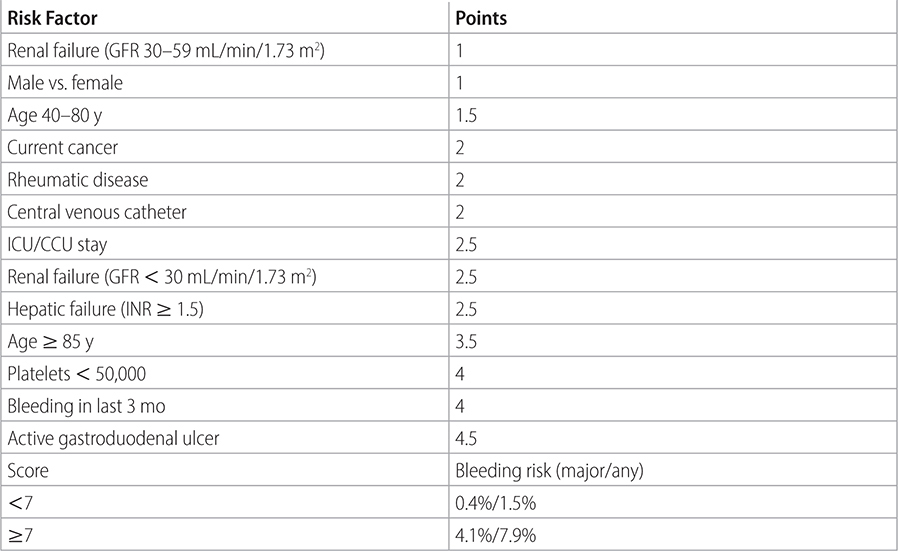
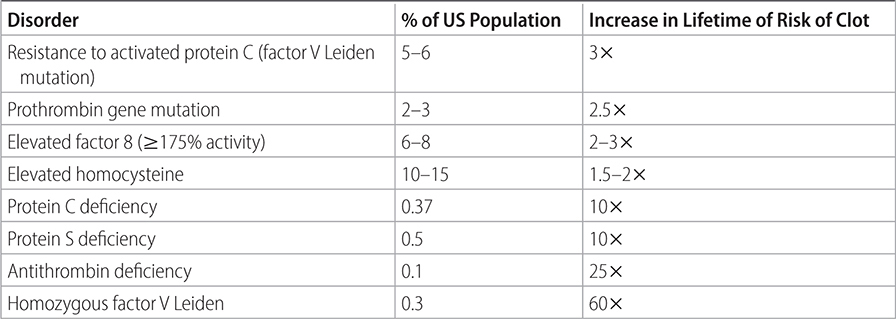
TABLE 2–9 HEREDITARY THROMBOPHILIC DISORDERS
Sources
–Blood Adv. 2018;2:3198-3225.
–American Society of Hematology 2018. Guidelines for Management of Venous Thromboembolism: Prophylaxis for Hospitalized and Nonhospitalized Medical Patients.
–JAMA. 2012;307:306.
–Ann Intern Med. 2011;155:625-632.
–Chest. 2016;149:315-352.
–http://www.uwhealth.org/files/uwheath/docs/anticoagulation/VTE
Population: Patients undergoing surgery.
Organization
 ACCP 2016
ACCP 2016
Prevention Recommendations
–Stratify surgical risk:
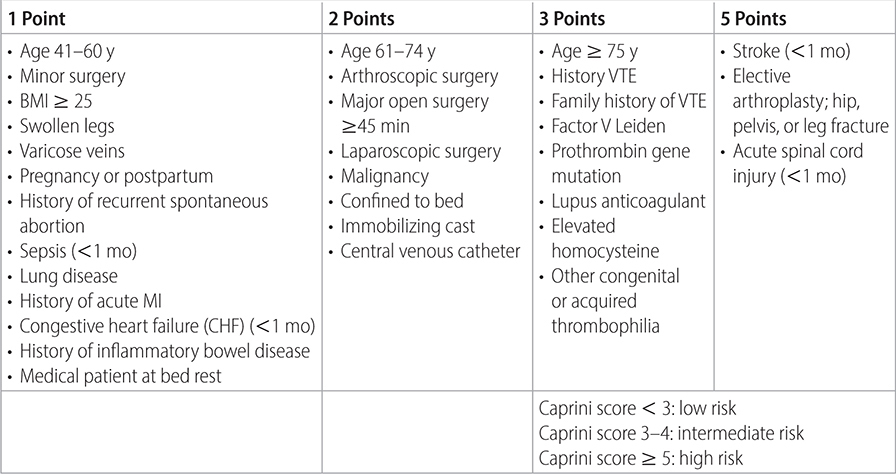
• Low risk: <40 y, minor surgery,1no risk factors,2Caprini score < 2 (Table 2–10).
• Intermediate risk: minor surgery plus risk factors, age 40–60 y, major surgery with no risk factors, Caprini score 3–4.
• High risk: major surgery plus risk factors, high-risk medical patient, major trauma, spinal cord injury, craniotomy, total hip or knee arthroplasty (THA, TKA), thoracic, abdominal, pelvic cancer surgery.
TABLE 2–10 CAPRINI RISK STRATIFICATION MODEL
–Employ preventive measures:
• Early ambulation: consider mechanical prophylaxis and IPC or GCS.
• UFH 5000 U SQ q 8–12 h should ONLY be used in patients with renal disease with a Ccr < 20–30 mL/min.
• LMWH equivalent to enoxaparin 40 mg SQ 2 h before surgery then daily or 30 mg q 12 h SQ starting 8–12 h postop.
• Fondaparinux 2.5 mg SQ daily starting 8–12 h postop.
• LMWH: equivalent to enoxaparin 40 mg SQ 2 h preoperative then daily or 30 mg SQ q 12 h starting 8–12 h postop and also use mechanical prophylaxis with IPC or GCS.
• Extend prophylaxis for as long as 28–35 d in high-risk patients. In THA, TKA ortho patients, acceptable VTE prophylaxis also includes rivaroxaban 10 mg/d, dabigatran 225 mg/d, adjusted dose warfarin, and aspirin, although LMWH is preferred. DOACs are likely to play a larger role in the future as trials continue to show superiority over warfarin. (Ann Int Med. 2013;159:275) (Thromb Haemot. 2011;105:444)
• If high risk of bleeding, use IPC alone. (Ann Intern Med. 2012;156:710, 720) (JAMA. 2012;307:294)
• Do not use UFH for prophylaxis if Ccr is ≥20 mL/min. There is a 10-fold increased risk of HIT compared to LMWH.
Practice Pearls
• 75%–90% of surgical bleeding is structural. VTE prophylaxis adds minimally to risk of bleeding.
• With creatinine clearance <20 to 30 mL/min UFH with partial thromboplastin time (PTT) monitoring is preferred (decrease dose if PTT is prolonged). In all other situations LMWH or DOACs are preferred to reduce the risk of HIT.
• Patients with liver disease and prolonged international normalized ratio (INR) are still at risk for clot. Individualize risk-to-benefit ratio of VTE prophylaxis.
• Epidural anesthesia: before placing catheter wait 18 h after daily prophylactic dose of LMWH and 24 h after prophylactic dose of fondaparinux. For patients on twice daily therapeutic LMWH anticoagulation or once daily LMWH, wait more than 24 h before placing epidural catheter. Patients on DOACs should hold their anticoagulation for 3–5 d. After placing or removing an epidural catheter hold on starting anticoagulation for 6–8 h.
• Do not place prophylactic IVC filter for high-risk surgery.
• For cranial and spinal surgery patients at low risk for VTE use mechanical prophylaxis: high-risk patients should have pharmacologic prophylaxis added to mechanical prophylaxis once hemostasis is established and bleeding risk decreased.
• Patients at high risk of bleeding1with major surgery should have mechanical prophylaxis (IPC, GCS): initiate anticoagulant prophylaxis if risk is lowered.
• Surgical patients receive indicated prophylaxis 60% of the time compared to 40% in medical patients.
Sources
–Chest. 2016;149:315.
–http://www.fda.gov/Drugs/ResourcesForYou/Consumers/ucm390574.htm