Absorption: Provides slower prolonged absorption and a relatively constant concentrations over 24 hr.
Distribution: Identical to endogenous insulin.
Half-Life: 5–6 min (prolonged in diabetic patients; biological half-life is longer).
(hypoglycemic effect)
| ROUTE | ONSET | PEAK | DURATION |
|---|---|---|---|
| SUBQ | 3–4 hr | none‡ | 24 hr |
‡Small amounts of insulin glargine are slowly released resulting in a relatively constant effect over time.
Contraindicated in:
Use Cautiously in:
Endo: HYPOGLYCEMIA
F and E: hypokalemia
Local: cutaneous amyloidosis, lipodystrophy, pruritus, erythema, swelling
Drug-drug:
Drug-Natural Products:
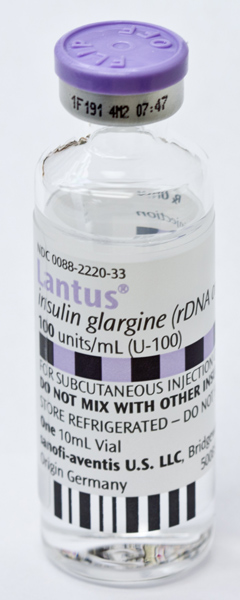
Toujeo has a lower glucose lowering effect than Basaglar, Lantus, Rezvoglar, or Semglee on a unit-to-unit basis.
Basaglar, Lantus, Rezvoglar, or Semglee
Toujeo
Lab Test Considerations:
Toxicity and Overdose:
Medication errors involving insulins have resulted in serious patient harm and death. Clarify all ambiguous orders and do not accept orders using the abbreviation “u” for units, which can be misread as a zero or the numeral 4 and has resulted in tenfold overdoses. Insulins are available in different types and strengths. Check type, dose, and expiration date with another licensed nurse. Do not interchange insulins without consulting health care professional. Do not confuse Lantus with Latuda. Do not confuse Toujeo with Tradjenta, Tresiba, or Trulicity
NDC Code