- General assessment and initial treatment
- Check blood pressure and pulse rate and rhythm. Perform cardiopulmonary resuscitation (CPR) if there is no pulse and perform advanced cardiac life support (ACLS) for dysrhythmias and shock. Note: Some ACLS drugs may be ineffective or dangerous in patients with drug- or poison-induced cardiac disorders. For example, type Ia antiarrhythmic drugs are contraindicated in patients with tricyclic antidepressant or other sodium channel-blocker overdose.
- Obtain a 12-lead ECG and begin continuous electrocardiographic (ECG) monitoring. Dysrhythmias may complicate a variety of drug overdoses, and all patients with potentially cardiotoxic drug poisoning should have an ECG and continuous cardiac monitoring in the emergency department or an intensive care unit for at least 6 hours after the ingestion. Prior ECGs are often useful for comparisons in those with pre-existing cardiac conditions.
- Secure venous access. Antecubital or forearm veins are usually easy to cannulate and large-caliber peripheral IV access allows for rapid fluid administration. Central venous access (eg, femoral, subclavian, internal jugular, and other central veins) is technically more difficult, but allows measurement of the central venous pressure and placement of a pacemaker or pulmonary artery lines. Intraosseous (IO) access may also be used in urgent situations.
- Draw blood for routine studies.
- Begin IV infusion of normal saline (NS), lactated Ringer's solutions (LR), 5% dextrose in NS (D5NS), 5% dextrose in half NS (D5W 0.45% sodium chloride), or 5% dextrose in water (D5W) at a keep-open rate; for children, use 5% dextrose in quarter NS (D5W 0.25% sodium chloride). If the patient is hypotensive, NS, LR, or another isotonic crystalloid solution is preferred.
- In seriously ill patients (eg, those who are hypotensive, obtunded, convulsing, or comatose), place a Foley catheter in the bladder, obtain urine for routine and toxicologic testing, and measure hourly urine output.
- Bradycardia and atrioventricular (AV) block
- Assessment. Examples of drugs and toxins causing bradycardia or AV block and their mechanisms are listed in Table I-4.
- Bradycardia and AV block are common features of intoxication with calcium antagonists and drugs that depress sympathetic tone (eg, clonidine, beta blockers) or increase parasympathetic tone (eg, digoxin). These conditions may also result from severe intoxication with sodium channel-blocking drugs (eg, tricyclic antidepressants, quinidine, and other types Ia and Ic antiarrhythmic agents).
- Bradycardia or AV block may also be a reflex response (baroreceptor reflex) to hypertension induced by alpha-adrenergic agents such as phenylpropanolamine and phenylephrine.
- In children, bradycardia is commonly caused by respiratory compromise and usually responds to ventilation and oxygenation.
- Complications. Bradycardia and AV block frequently cause hypotension, which may progress to asystolic cardiac arrest.
- Differential diagnosis. Rule out the following:
- Hypothermia.
- Myocardial ischemia or infarction.
- Electrolyte abnormality (eg, hyperkalemia).
- Metabolic disturbance (eg, hypothyroidism).
- Physiologic origin, resulting from a baroreceptor response to hypertension, an intrinsically slow pulse rate (common in athletes), or an acute vasovagal reaction.
- Cushing reflex (caused by severe intracranial hypertension).
- Treatment. Do not treat bradycardia or AV block unless the patient is symptomatic (eg, exhibits signs of syncope or hypotension). Note: Bradycardia or even AV block may be a protective baroreceptor reflex to lower the blood pressure in a patient with severe hypertension (see Item VII below).
- Maintain an open airway and assist ventilation (Airway) if necessary. Administer supplemental oxygen.
- Rewarm hypothermic patients. A sinus bradycardia of 40-50 beats/min is common when the body temperature is 32-35°C (90-95°F) and will usually return to normal with warming.
- Administer atropine, 0.01-0.03 mg/kg IV. If this is not successful, use isoproterenol, 1-10 mcg/min IV, titrated to the desired rate, or use an emergency transcutaneous or transvenous pacemaker.
- Use the following specific interventions if appropriate:
- For beta receptor antagonist overdose, give glucagon.
- For digoxin, digitalis, or other cardiac glycoside intoxication, use Fab antibody fragments.
- For tricyclic antidepressant or membrane-depressant drug overdose, administer sodium bicarbonate.
- For calcium antagonist overdose, give calcium, hyperinsulin-euglycemia therapy, or lipid emulsion.
- Assessment. Examples of drugs and toxins causing bradycardia or AV block and their mechanisms are listed in Table I-4.
- QRS interval prolongation
- Assessment. Normal QRS interval is 80-100 msec. Examples of drugs and toxins causing QRS interval prolongation are listed in Table I-5.
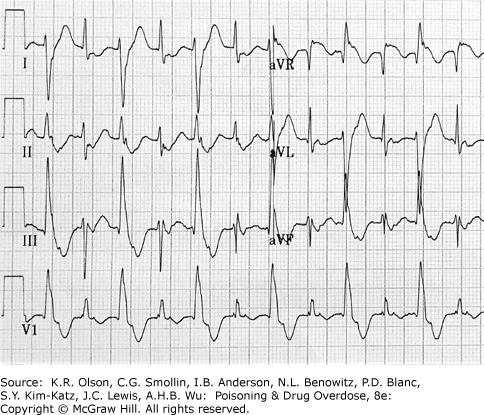
- QRS interval prolongation of greater than 100 msec in the limb leads (Figure I-2) is common in poisoning by tricyclic antidepressants or other membrane-depressant drugs (eg, quinidine, flecainide (Antiarrhythmic Drugs), chloroquine, and propranolol (Beta-Adrenergic Blockers). Rightward axis deviation of the terminal 40 msec of the ECG, recognized as a late R wave in the aVR lead, may precede QRS widening (Figure I-3).
- QRS interval prolongation may also result from a ventricular escape rhythm in a patient with complete heart block (eg, from digitalis, calcium antagonist poisoning, or intrinsic cardiac disease).
- Complications. QRS interval prolongation in patients with tricyclic antidepressant or similar drug poisoning is often accompanied by hypotension, AV block, and seizures. Widening of QRS beyond 160 msec is associated with an increased likelihood of ventricular arrhythmias (ventricular tachycardia, bigeminy, idioventricular rhythm) and shock.
- Differential diagnosis. Rule out the following:
- Intrinsic conduction system disease (bundle branch block or complete heart block). Check an old ECG if available.
- Brugada syndrome, an inherited disorder associated with sudden cardiac death.
- Hyperkalemia with critical cardiac toxicity may appear as a “sine wave” pattern with markedly wide QRS complexes. These are usually preceded by peaked T waves (Figure I-4).
- Hypothermia with a core temperature of less than 32°C (90°F) often causes an extraterminal QRS deflection (J wave or Osborne wave), resulting in a widened QRS appearance (Figure I-5).
- Treatment
- For tricyclic antidepressant or other sodium channel-blocking drug overdose, give sodium bicarbonate, 1- to 2-mEq/kg IV bolus; repeat as needed. Refractory QRS widening may require hypertonic saline, lipid emulsion therapy, or lidocaine.
- Maintain the airway and assist ventilation if necessary (Airway). Administer supplemental oxygen.
- Treat hyperkalemia and hypothermia if they occur.
- Treat AV block with atropine, isoproterenol, and a pacemaker if necessary.
- Assessment. Normal QRS interval is 80-100 msec. Examples of drugs and toxins causing QRS interval prolongation are listed in Table I-5.
- Tachycardia
- Assessment. Examples of drugs and toxins causing tachycardia and their mechanisms are listed in Table I-6.
- Sinus tachycardia and supraventricular tachycardia are often caused by excessive sympathetic stimulation or inhibition of parasympathetic tone. Sinus tachycardia may also be a reflex response to hypotension or hypoxia.
- Sinus tachycardia and supraventricular tachycardia accompanied by QRS interval prolongation (eg, with tricyclic antidepressant poisoning) may have the appearance of ventricular tachycardia (see Figure I-2).
- Complications. Simple sinus tachycardia (heart rate <140 beats/min) is rarely of hemodynamic consequence; children and healthy adults easily tolerate rates of up to 160-180 beats/min. However, sustained rapid rates may result in hypotension, chest pain, myocardial ischemia, or syncope.
- Differential diagnosis. Rule out the following:
- Occult blood loss (eg, from gastrointestinal bleeding or trauma).
- Fluid loss (eg, third spacing, gastroenteritis).
- Hypoxia.
- Fever and infection.
- Hyperthyroidism.
- Anxiety or untreated pain.
- Intrinsic conduction system disease (eg, Wolff-Parkinson-White syndrome) causing tachydysrhythmia.
- Treatment. Identification and treatment of the underlying cause is the single most important intervention. If tachycardia is not associated with hypotension or chest pain, observation and sedation with benzodiazepines (especially for stimulant intoxication) are usually adequate.
- Sympathomimetic-induced tachycardia resulting in ischemia or rate-related hypotension: give a short-acting, titratable beta blocker such as esmolol, 0.025-0.1 mg/kg/min IV. Note: If tachycardia is accompanied by hypertension, add a vasodilator (see Item VII.D.2 below).
- Anticholinergic-induced tachycardia may respond to physostigmine or neostigmine, but tachycardia alone is rarely an indication for use of these drugs.
- Assessment. Examples of drugs and toxins causing tachycardia and their mechanisms are listed in Table I-6.
- Ventricular dysrhythmias
- Assessment. Examples of drugs and toxins causing ventricular dysrhythmias are listed in Table I-7.
- Ventricular irritability is commonly associated with excessive sympathetic stimulation (eg, from cocaine or amphetamines). Patients intoxicated by chlorinated, fluorinated, or other hydrocarbons may have heightened myocardial sensitivity to the arrhythmogenic effects of catecholamines.
- Ventricular tachycardia can also occur in overdose of tricyclic antidepressants and other sodium channel-blocking drugs, although true ventricular tachycardia may be difficult to distinguish from sinus or supraventricular tachycardia accompanied by QRS interval prolongation (see Figure I-2).
- Bidirectional ventricular tachycardia (see Figure I-6) is a rare ventricular arrhythmia seen in some patients with cardiac glycoside or aconitine toxicity.
- Agents that cause QT interval prolongation (QTc >0.43 seconds in men, >0.45 seconds in women) may produce torsade de pointes. Torsade de pointes is a polymorphous ventricular tachycardia in which the axis appears to rotate continuously (Figure I-7). Torsade de pointes may also be caused by hypokalemia, hypocalcemia, or hypomagnesemia.
- Complications. Ventricular tachycardia in patients with a pulse may be associated with hypotension or may deteriorate into pulseless ventricular tachycardia or ventricular fibrillation.
- Differential diagnosis. Rule out the following possible causes of ventricular premature beats, ventricular tachycardia, or ventricular fibrillation:
- Hypoxemia.
- Hypokalemia.
- Metabolic acidosis.
- Myocardial ischemia or infarction.
- Electrolyte disturbances (eg, hypocalcemia or hypomagnesemia) or congenital disorders that may cause QT prolongation and torsade de pointes.
- Brugada syndrome.
- Treatment. Perform CPR if necessary and follow standard ACLS guidelines for the management of dysrhythmias, with the exception that type Ia antiarrhythmic drugs should not be used, especially if tricyclic antidepressant or sodium channel-blocking drug overdose is suspected.
- Maintain an open airway and assist ventilation if necessary (Airway). Administer supplemental oxygen.
- Correct acid-base and electrolyte disturbances.
- For myocardial sensitivity caused by hydrocarbons (eg, chloral hydrate, halogenated or aromatic hydrocarbons), use an easily titratable and short-acting beta-blocker such as esmolol, 0.025-0.1 mg/kg/min IV.
- For ventricular dysrhythmias due to tricyclic antidepressant or other sodium channel-blocking drug overdose, administer sodium bicarbonate, 1-2 mEq/kg IV in repeated boluses until the dysrhythmia is interrupted and QRS interval narrows to less than 160 msec or the serum pH exceeds 7.55. Hypertonic saline (3% sodium chloride given as 1-2 mEq/kg bolus), lipid emulsion, lidocaine, and extracorporeal membrane oxygenation (ECMO) may also be considered.
- For polymorphic ventricular tachycardia (torsade de pointes), do the following:
- Administer IV magnesium sulfate, 1-2 g in adults, over 20-30 minutes.
- Use overdrive pacing or isoproterenol, 1-10 mcg/min IV, to increase the heart rate (this makes repolarization more homogeneous and abolishes the dysrhythmia).
- As with other types of ventricular dysrhythmias, immediate defibrillation is warranted if the patient is unstable or pulseless.
- Assessment. Examples of drugs and toxins causing ventricular dysrhythmias are listed in Table I-7.
- Hypotension
- Assessment. Examples of drugs and toxins causing hypotension and their mechanisms are listed in Table I-8.
- Physiologic derangements resulting in hypotension include volume loss due to vomiting, diarrhea, or bleeding; apparent volume depletion caused by venodilation, arteriolar dilation, depression of cardiac contractility, and dysrhythmias that interfere with cardiac output; and hypothermia.
- Check the pulse rate. Volume loss, venodilation, and arteriolar dilation are likely to result in hypotension with reflex tachycardia. In contrast, hypotension accompanied by bradycardia should suggest intoxication by sympatholytic agents, membrane-depressant drugs, calcium antagonists, or cardiac glycosides, or the presence of hypothermia.
- Bedside ultrasound can help guide resuscitation through rapid determination of cardiac contractility and intravascular volume status. It may also help exclude alternative diagnoses.
- Complications. Severe or prolonged hypotension can cause acute renal tubular necrosis, brain damage, hepatic and gastrointestinal necrosis, and cardiac ischemia. Metabolic acidosis is a common finding.
- Differential diagnosis. Rule out the following:
- Hypothermia, which results in a decreased metabolic rate and lowered blood pressure demands.
- Hyperthermia, which causes arteriolar dilation and venodilation and direct myocardial depression.
- Fluid loss caused by gastroenteritis.
- Blood loss (eg, from trauma or gastrointestinal bleeding).
- Myocardial infarction or cardiomyopathy.
- Sepsis.
- Spinal cord injury.
- Treatment. Fortunately, hypotension usually responds readily to empiric therapy with IV fluids and low doses of vasoactive drugs (eg, dopamine, norepinephrine). When hypotension does not resolve after simple measures, a systematic approach should be followed to determine the cause of hypotension and select the appropriate treatment.
- Maintain an open airway and assist ventilation if necessary (Airway). Administer supplemental oxygen.
- Treat cardiac dysrhythmias that may contribute to hypotension (heart rate <40-50 beats/min or >180-200 beats/min).
- Hypotension associated with hypothermia often will not be relieved unless the patient is rewarmed. A systolic blood pressure of 80-90 mm Hg is expected when the body temperature is 32°C (90°F).
- Give an IV fluid challenge with isotonic crystalloids, 10-20 mL/kg.
- Administer vasopressors. The choice of vasopressor depends upon the etiology of hypotension (eg, cardiogenic vs. vasodilatory shock).
- A direct-acting vasopressor such as norepinephrine, 0.1 mcg/kg/min IV, or phenylephrine may be more effective in patients with alpha-adrenergic receptor blockade (eg, tricyclic antidepressants, phenothiazines).
- An indirect vasopressor such as dopamine, 5-15 mcg/kg/min, can increase heart rate and contractility. It may be ineffective in some patients with depleted catecholamines (eg, from disulfiram or tricyclic antidepressant overdose).
- Vasopressin, or antidiuretic hormone, is commonly added as an adjunctive pressor agent to reverse vasodilatory shock.
- Consider specific antidotes for some toxins:
- Sodium bicarbonate for tricyclic antidepressant or other sodium channel-blocking drug overdose.
- Glucagon for beta receptor antagonist overdose.
- Calcium for calcium antagonist overdose.
- Propranolol or esmolol may reverse hypotension associated with theophylline, caffeine, or albuterol or other beta agonist overdose (because these agents cause peripheral vasodilation mediated through beta2 receptors).
- Clonidine toxicity may, in some cases, respond to naloxone administration, but the magnitude of effect is unpredictable.
- Other drug treatments:
- Severe hypotension due to calcium antagonist or beta blocker poisoning may respond to hyperinsulin-euglycemia therapy.
- Lipid emulsion may be useful for severe cardiotoxicity due to lipid-soluble drugs (eg, bupivacaine, verapamil, bupropion).
- If adrenal insufficiency is suspected, administer corticosteroids (eg, hydrocortisone, 100 mg IV every 8 hours).
- Methylene blue or hydroxocobalamin may increase blood pressure in poisoned patients with vasodilatory shock, by decreasing nitric oxide synthesis.
- Naloxone may act to support blood pressure by antagonizing endorphin-mediated effects on vascular tone.
- If empiric measures to restore the blood pressure are unsuccessful, assess volume status and cardiac contractility with bedside ultrasound, or insert a central venous pressure (CVP) monitor or pulmonary artery catheter. Although invasive, CVP monitoring can help to determine whether further IV fluids are needed and to measure the cardiac output (CO) and calculate the systemic vascular resistance (SVR):
Select further therapy on the basis of the following:
- If the central venous pressure or pulmonary artery wedge pressure remains low, give more IV fluids.
- If the cardiac output is low, give more dopamine or dobutamine.
- If the systemic vascular resistance is low, administer norepinephrine, 4-8 mcg/min, or phenylephrine.
- Patients refractory to medical interventions may benefit from extracorporeal membrane oxygenation (ECMO, or “heart-lung bypass”), which helps to perfuse the vital organs until the toxin can be eliminated or metabolized.
- Assessment. Examples of drugs and toxins causing hypotension and their mechanisms are listed in Table I-8.
- Hypertension
- Assessment. Hypertension is frequently overlooked in drug-intoxicated patients and often goes untreated. Many young people have normal blood pressures in the range of 90/60-100/70 mm Hg; in such a person, an abrupt elevation to 170/100 mm Hg is much more significant (and potentially catastrophic) than the same blood pressure elevation in an older person with chronic hypertension. Examples of drugs and toxins causing hypertension are listed in Table I-9. Hypertension may be caused by a variety of mechanisms:
- Amphetamines and other related drugs cause hypertension and tachycardia through generalized sympathetic stimulation.
- Selective alpha-adrenergic agents cause hypertension with reflex (baroreceptor-mediated) bradycardia or even AV block.
- Anticholinergic agents cause mild hypertension with tachycardia.
- Substances that stimulate nicotinic cholinergic receptors (eg, organophosphates) may initially cause tachycardia and hypertension, followed later by bradycardia and hypotension.
- Withdrawal from sedative-hypnotic drugs, ethanol, opioids, or clonidine can cause hypertension and tachycardia.
- Complications. Severe hypertension can result in intracranial hemorrhage, aortic dissection, myocardial infarction, renal injury, and congestive heart failure.
- Differential diagnosis. Rule out the following:
- Idiopathic hypertension (which is common in the general population). However, without a prior history of hypertension, it should not be initially assumed to be the cause of the elevated blood pressure.
- Pheochromocytoma or other paraganglionic tumors that secrete epinephrine, norepinephrine, or both are rare but potentially lethal. They typically cause paroxysmal attacks of hypertension, headache, perspiration, and palpitations.
- Increased intracranial pressure caused by spontaneous hemorrhage, trauma, or other causes. This may result in hypertension with reflex bradycardia (Cushing reflex).
- Treatment. Rapid lowering of the blood pressure is desirable as long as it does not result in hypotension, which can potentially cause an ischemic cerebral infarction in older patients with cerebrovascular disease. For a patient with chronic hypertension, lowering the diastolic pressure to 100 mm Hg is acceptable. However, for a young person whose normal diastolic blood pressure is 60 mm Hg, the diastolic pressure should be lowered to 80 mm Hg.
- For hypertension with little or no tachycardia, vasodilator treatment is recommended. Use phentolamine, 0.02-0.1 mg/kg IV, or nitroprusside, 2-10 mcg/kg/min IV.
- For hypertension with tachycardia, add a beta blocker to the vasodilator treatment in Item 1 above. Give esmolol, 0.025-0.1 mg/kg/min IV, or labetalol, 0.2-0.3 mg/kg IV. Caution: Do not use beta blockers without a vasodilator to treat hypertensive crisis; beta receptor antagonists may paradoxically worsen hypertension because any alpha-mediated vasoconstriction is unopposed when beta2-mediated vasodilation is blocked. Although labetalol has some alpha-adrenergic receptor blocker activity, it may be insufficient to overcome unopposed alpha effects.
- If hypertension is accompanied by a focally abnormal neurologic examination (eg, hemiparesis), perform computed tomography (CT) as quickly as possible. In a patient with a cerebrovascular accident, hypertension should generally not be treated unless specific complications of the elevated pressure (eg, heart failure or cardiac ischemia) are present. Consult a neurologist or neurosurgeon.
- Assessment. Hypertension is frequently overlooked in drug-intoxicated patients and often goes untreated. Many young people have normal blood pressures in the range of 90/60-100/70 mm Hg; in such a person, an abrupt elevation to 170/100 mm Hg is much more significant (and potentially catastrophic) than the same blood pressure elevation in an older person with chronic hypertension. Examples of drugs and toxins causing hypertension are listed in Table I-9. Hypertension may be caused by a variety of mechanisms:
Cholinergic or vagotonic agents Digitalis glycosides Organophosphates and carbamates Physostigmine, neostigmine Membrane-depressant drugs Propranolol Encainide and flecainide Quinidine and other type Ia antidysrhythmics Tricyclic antidepressants
| Sympatholytic agents Beta receptor antagonists Clonidine Opioids Other Calcium antagonists Carbamazepine Grayanotoxin (“mad honey”) Ivabradine Lithium Phenylpropanolamine and other alpha-adrenergic agonists |
aReprinted by permission from the Springer Nature: Med Toxicol. 2,52-81; Physical assessment and differential diagnosis of the poisoned patient, Olson KR, et al. ©1987.
| Bupropion | Lamotrigine |
| Chloroquine and related agents | Phenothiazines (thioridazine) |
| Cocaine (high-dose) | Propoxyphene |
| Digitalis glycosides (complete heart block) | Propranolol |
| Diphenhydramine (high-dose) | Quinidine and other type Ia antidysrhythmics |
| Encainide and flecainide | Tricyclic antidepressants |
| Hyperkalemia | Venlafaxine |
aReprinted by permission from the Springer Nature: Med Toxicol. 2,52-81; Physical assessment and differential diagnosis of the poisoned patient, Olson KR, et al. ©1987.
FIGURE I-2. Widened QRS Interval Caused by Tricyclic Antidepressant Overdose
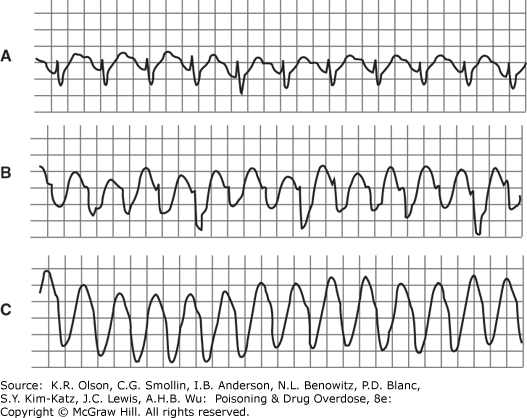
Widened QRS interval caused by tricyclic antidepressant overdose. A: Delayed intraventricular conduction results in prolonged QRS interval (0.18 s). B and C: Supraventricular tachycardia with progressive widening of QRS complexes mimics ventricular tachycardia. (Reproduced with permission from Benowitz NL et al. Cardiac disturbances in the toxicologic patient. In: Haddad LM, Winchester JF, eds. Clinical Management of Poisoning and Drug Overdose, WB Saunders/Elsevier, 3rd ed., 1998.)
FIGURE I-3. Right Axis Deviation of the Terminal 40 msec, Easily Recognized As a Late R Wave in aVR
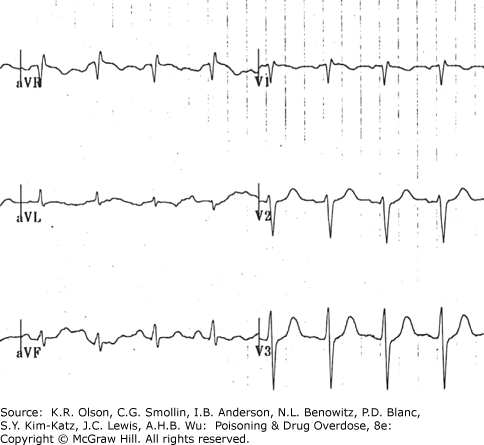
Right axis deviation of the terminal 40 msec, easily recognized as a late R wave in aVR.
FIGURE I-4. Electrocardiogram of a Patient with Hyperkalemia
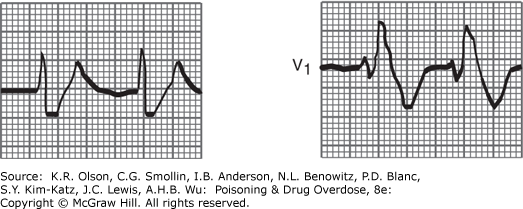
Electrocardiogram of a patient with hyperkalemia. (Reproduced with permission from Goldschlager N, Goldman MJ. Effect of drugs and electrolytes on the electrocardiogram. In: Goldschlager N, Goldman MJ, eds. Electrocardiography: Essentials of Interpretation, New York; Appleton & Lange (McGraw Hill); 1984, p 199.)
FIGURE I-5. Electrocardiogram of a Patient with Hypothermia, Showing Prominent J Waves
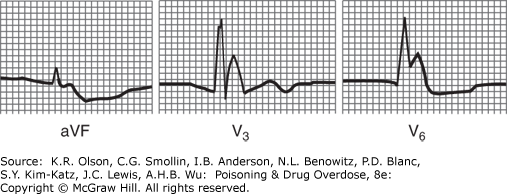
Electrocardiogram of a patient with hypothermia, showing prominent J waves. (Reproduced with permission from Goldschlager N, Goldman MJ. Effect of drugs and electrolytes on the electrocardiogram. In: Goldschlager N, Goldman MJ, eds. Electrocardiography: Essentials of Interpretation, New York; Appleton & Lange (McGraw Hill);1984, p 227).
Sympathomimetic agents Amphetamines and derivatives Caffeine Cocaine Ephedrine and pseudoephedrine Phencyclidine (PCP) Theophylline Agents causing cellular hypoxia Carbon monoxide Cyanide Hydrogen sulfide Oxidizing agents (methemoglobinemia) | Anticholinergic agents Amanita muscaria mushrooms Antihistamines Atropine and other anticholinergics Phenothiazines Plants (many Plants) Tricyclic antidepressants Other Ethanol, sedative-hypnotic, or opioid drug withdrawal Vasodilators (reflex tachycardia) Thyroid hormone |
aReprinted by permission from the Springer Nature: Med Toxicol. 2,52-81; Physical assessment and differential diagnosis of the poisoned patient, Olson KR, et al. ©1987.
| Ventricular tachycardia or fibrillation | |
Aconitine Amphetamines and other sympathomimetic agents Aromatic hydrocarbons/inhalants Barium Bupropion Caffeine and theophylline Chloral hydrate Chlorinated or fluorinated hydrocarbon solvents | Cocaine Digitalis glycosides Fluoride/hydrofluoric acid Grayanotoxin (“mad honey”) Lamotrigine Phenothiazines Theophylline Tricyclic antidepressants |
| QT prolongation with documented risk for torsade de pointesb | |
Amiodarone Arsenic trioxide Azithromycin Bepridil Cesium Chloroquine Chlorpromazine Ciprofloxacin Clarithromycin Cocaine Disopyramide Dofetilide Donepezil Droperidol Erythromycin Escitalopram Flecainide Fluconazole Haloperidol Hydroxychloroquine | Ibutilide Levofloxacin Loperamide (high dose) Metoclopramide Methadone Moxifloxacin Ondansetron Pentamidine Pimozide Propofol Procainamide Organophosphate insecticides Quinidine Sevoflurane Sotalol Thallium Thioridazine
|
aOlson KR. et al. Med Toxicol. 1987;2:71; and https://www.crediblemeds.org. Accessed December 4, 2020.
bTorsade de pointes can deteriorate into ventricular fibrillation and cardiac arrest.
FIGURE I-6. Electrocardiogram of a Patient with Bidirectional Ventricular Tachycardia Due to Aconite Poisoning
Electrocardiogram of a patient with bidirectional ventricular tachycardia due to aconite poisoning. ECG courtesy of Craig Smollin, MD.
FIGURE I-7. Polymorphic Ventricular Tachycardia (Torsade De Pointes)
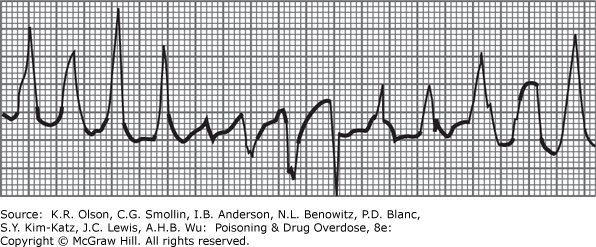
Polymorphic ventricular tachycardia (torsade de pointes). (Reproduced with permission from Goldschlager N, Goldman MJ. Effect of drugs and electrolytes on the electrocardiogram. In: Goldschlager N, Goldman MJ, eds. Electrocardiography: Essentials of Interpretation, New York; Appleton & Lange (McGraw Hill); 1984, p 197.)
HYPOTENSION WITH RELATIVE BRADYCARDIA Sympatholytic agents Beta receptor antagonists Clonidine and methyldopa Hypothermia Opioids Reserpine Tetrahydrozoline and oxymetazoline Membrane-depressant drugs Bupropion Encainide and flecainide Quinidine, procainamide, and disopyramide Propoxyphene Propranolol Tricyclic antidepressants Others Barbiturates Calcium antagonists (verapamil, diltiazem) Cyanide Fluoride Hydrogen sulfide Organophosphates and carbamates Sedative-hypnotic agents Tilmicosin | HYPOTENSION WITH TACHYCARDIA Fluid loss or third spacing Amatoxin-containing mushrooms Arsenic Colchicine Copper sulfate Corrosive/caustic ingestion Glyphosate/ surfactant herbicides Hyperthermia Iron Paraquat/diquat Rattlesnake envenomation Sedative-hypnotic agents
Peripheral venous or arteriolar dilation Alpha antagonists (doxazosin, prazosin, terazosin) Beta2 receptor agonists (eg, albuterol) Caffeine and theophylline Calcium antagonists (nifedipine, amlodipine, nicardipine) Cyanide Disulfiram Ethanol Hydralazine Hyperthermia Minoxidil Nitrites Sodium nitroprusside Phosphides Phenothiazines Quetiapine Scombroid Tricyclic antidepressants |
aReprinted by permission from the Springer Nature: Med Toxicol. 2,52-81; Physical assessment and differential diagnosis of the poisoned patient, Olson KR, et al. ©1987.
| HYPERTENSION WITH TACHYCARDIA | |
Generalized sympathomimetic agents Amphetamines and derivatives Cocaine Ephedrine and pseudoephedrine Epinephrine Levodopa LSD (lysergic acid diethylamide) Marijuana Monoamine oxidase inhibitors Synthetic cathinones and cannabinoids | Anticholinergic agentsb Antihistamines Atropine and other anticholinergics Tricyclic antidepressants Others Ethanol and sedative-hypnotic drug withdrawal Nicotine (early stage) Organophosphates (early stage)
|
| HYPERTENSION WITH BRADYCARDIA OR ATRIOVENTRICULAR BLOCK | |
Clonidine, tetrahydrozoline, and oxymetazolinec | Norepinephrine |
Ergot derivatives | Phenylephrine |
Methoxamine | Phenylpropanolamine |
aReprinted by permission from the Springer Nature: Med Toxicol. 2,52-81; Physical assessment and differential diagnosis of the poisoned patient, Olson KR, et al. ©1987.
bHypertension is usually mild and associated with therapeutic or slightly supratherapeutic levels. Overdose may cause hypotension, especially with tricyclics.
cHypertension is often transient and followed by hypotension.