B.4. A limited bedside transthoracic echocardiogram is performed, demonstrating a layer of clotted blood anterior to the right atrium (RA) and ventricle. What echocardiographic findings support the diagnosis of cardiac tamponade?
Answer:
It is important to emphasize that cardiac tamponade is a clinical diagnosis, characterized by clinical deterioration (shortness of breath in the supine or even sitting position, worsening shock with low SV) and supported by echocardiographic findings.
A key concept when interpreting imaging in a patient with suspected cardiac tamponade is that the size of a pericardial effusion does not correspond to the severity of clinical symptoms; a small acute pericardial effusion can cause life-threatening cardiac tamponade but remain occult on imaging. For example, the presence of mediastinal clot is an anatomical finding that might simply reflect a postsurgical state. Echocardiographic findings that correspond to the pathophysiology of cardiac tamponade in this patient include the following:
Increased intrapericardial pressures causing diastolic collapse of the atria and/or right ventricle. The RA is most sensitive to compression just after the atrial kick (ie, P wave on electrocardiogram [ECG]), when atrial pressure is lowest (Figure 12.7). The period of collapse extends further through the cardiac cycle with increasing pericardial pressures, so that right atrial collapse exceeding one-third of the cardiac cycle is nearly 100% sensitive and specific for cardiac tamponade. The RV, with a higher chamber pressure than the atria, is less susceptible to compression, but the finding of RV diastolic collapse remains a highly specific sign of cardiac tamponade. The RV is most sensitive to compression in early diastole (ie, after T wave on ECG), when its chamber pressure is lowest.
Figure 12.7.: Right Atrium (RA) Collapse from Early Cardiac Tamponade.
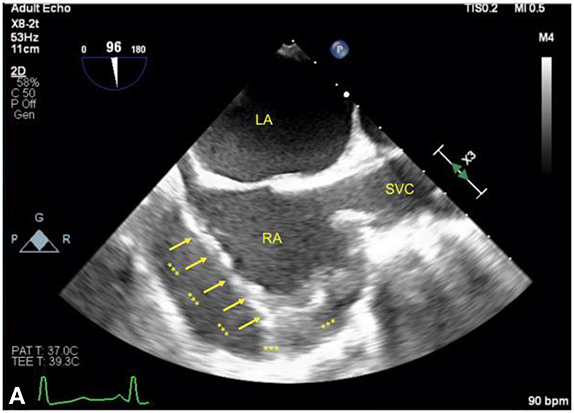
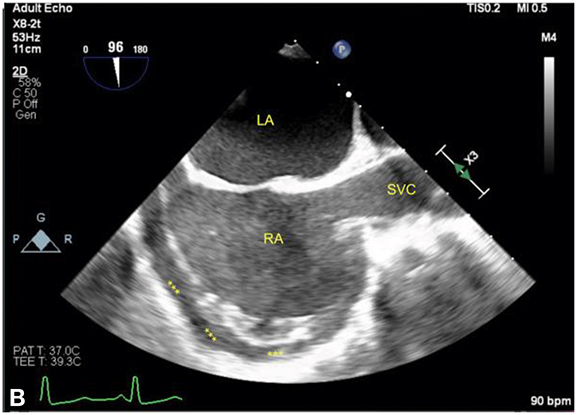
Right atrium (RA) collapse from early cardiac tamponade. The figures show the RA in the midesophageal bicaval view in the same patient with an acute pericardial effusion (labeled with asterisks). A. The RA is compressed by the effusion (arrows) in early ventricular systole as denoted by the ECG, corresponding approximately to the x-descent on a CVP waveform when the RA is most susceptible to compression. B. The RA in late ventricular systole is seen, corresponding to a point just before the V-wave, when the atrium is at its fullest just before tricuspid valve opening. LA, left atrium; SVC, superior vena cava.
Exaggerated ventricular interdependence. Doppler interrogation of mitral and tricuspid inflow velocities demonstrates increased RV filling and decreased LV filling during spontaneous inspiration. This increased RV filling causes a ventricular septal "bounce" toward the LV as RV free wall expansion meets pericardial constraint. Pulsed-wave Doppler of tricuspid inflow shows an increase in peak E-wave velocity by 40% compared with expiration, whereas mitral inflow shows a 25% inspiratory decrease in peak E-wave velocity (Figure 12.8). Venous inflow to the RA can also be interrogated via pulsed-wave Doppler of the hepatic vein, which initially shows systolic blunting of systolic velocities, with increased respiratory variation in diastolic velocity best seen by transesophageal echocardiography (TEE) or CVP tracing (Figure 12.5). In critical cardiac tamponade, diastolic velocities can be near-absent except during spontaneous inspiration or mechanical expiration.
Figure 12.8.: Exaggerated Ventricular Interdependence.
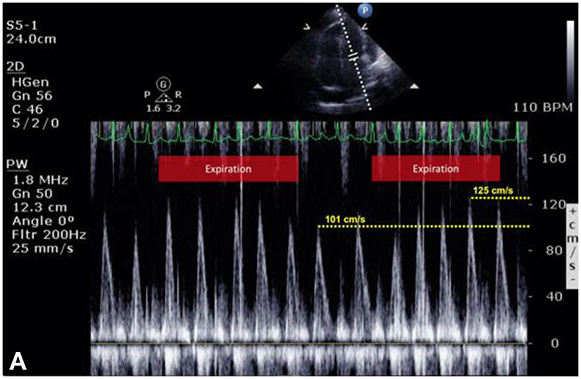
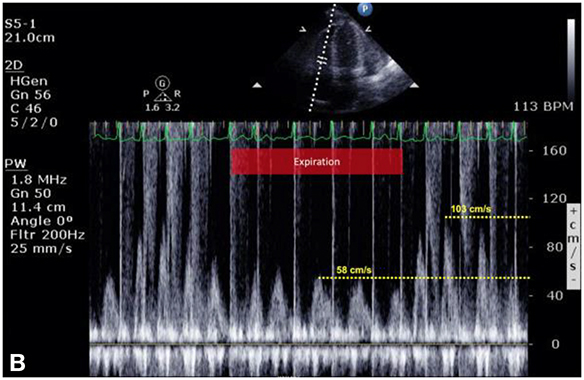
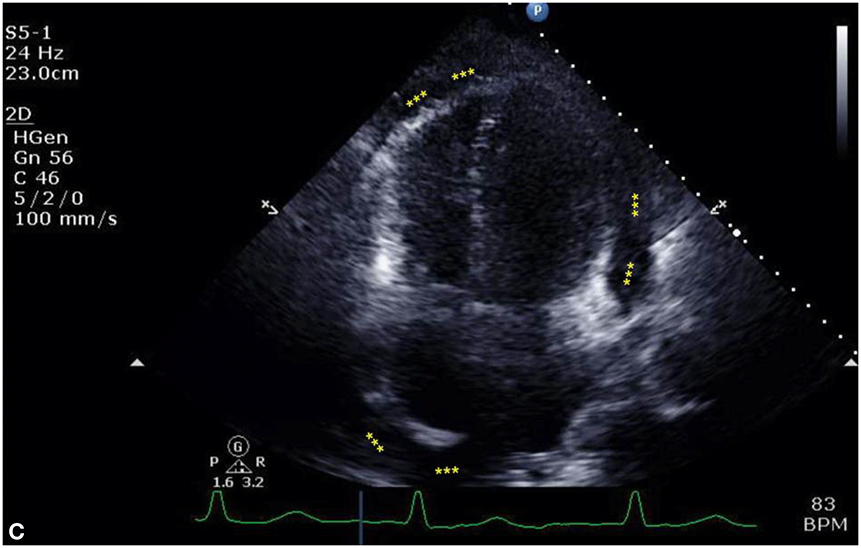
Exaggerated ventricular interdependence. A and B show pulsed-wave Doppler interrogation of transmitral and transtricuspid velocities obtained during a transthoracic echocardiographic study in a patient with suspected cardiac tamponade. The patient is breathing spontaneously; although there is no respirogram on the original images, the patient's marked sinus arrhythmia clearly defines inspiratory and expiratory phases. During negative pressure inspiration, A demonstrates a 25% decrease in transmitral E-wave velocities, whereas B shows a more than 45% increase in transtricuspid E-wave velocities. This exaggerated, reciprocal change in ventricular filling is a hallmark of cardiac tamponade and constrictive physiology. C shows an apical four-chamber view of this patient's heart, demonstrating a large effusion outside the right and left ventricles as well as a deep pool surrounding the right atrium (RA) (labeled by asterisks). Although not evident on this still image, interventricular septal "bounce" was prominent.
Decreased volume within cardiac chambers. This is suggested by decreased LV cavity size and exaggerated interatrial septal motion (in the presence of a high measured CVP) reflecting low transmural LA and RA pressures and abnormal ventricular filling patterns due to increased interdependence. The IVC can be distended due to obstructed venous return.
References
- Carmona P, Mateo E, Casanovas I, et al. Management of cardiac tamponade after cardiac surgery. J Cardiothorac Vasc Anesth. 2012;26:302-311.
- Ellenbroek DFJ, van Kessel L, Compagner W, et al. Diagnostic performance of echocardiography to predict cardiac tamponade after cardiac surgery. Eur J Cardiothorac Surg. 2022;62:ezab468.
- Gillam LD, Guyer DE, Gibson TC, et al. Hydrodynamic compression of the right atrium: a new echocardiographic sign of cardiac tamponade. Circulation. 1983;68:294-301.


