C.1. What are the surgical approaches to thoracic aneurysm repair?
Answer:
Ascending Aortic Aneurysms
Proximal ascending aneurysms not only cause aortic rupture and dissection but can also alter the three-dimensional conformation of the aortic root and/or AV, leading to AI (Figure 9.1). The extent of aortic root involvement determines the surgical procedure necessary for repair (Table 9.3). Repair with a supracoronary tube graft is indicated for patients who have ascending aortic aneurysms distal to the aortic root. The Wheat procedure is performed when the AV and proximal aorta are diseased without dilatation of the aortic root. It involves AV and supracoronary tube graft replacement, but spares the aortic root and, therefore, does not require reimplantation of the coronary arteries. When an ascending aortic repair involves the aortic root, various procedures can be performed depending on whether the architecture of the AV is preserved. If the AV is diseased, the Bentall procedure is performed to replace both the AV and root as well as reimplant the coronary arteries with a collar of the normal surrounding aorta, termed coronary buttons, onto the neoaorta. If atherosclerosis or dissection preclude proximal coronary arteries or aorta from being suitable for creating an anastomosis, the Cabrol technique can be used to fashion a conduit that typically extends the anastomoses to more distal portions of the coronary arteries. However, if the AV is not diseased, valve-sparing modifications of the Bentall technique can be performed to preserve the flow dynamics of the native AV and avoid the need for anticoagulation. David repairs, the most common type of valve-sparing procedures, entail replacement of excised native aorta with a graft in which the native AV is resuspended; the aortic graft used in David repairs is typically sutured below the AV insertion site, thus preventing further dilatation of the aortic root and thereby decreasing AI. An older valve-sparing technique, known as the Yacoub repair, aims to reconstruct the aorta with a scalloped graft that recreates neo-sinuses of Valsalva and attaches above the AV plane.
Table 9.3: Types of Thoracic Ascending Aorta Aneurysm Repairs
| Aortic Valve | Root | Ascending Aorta | Surgical Approach | Name of Procedure |
|---|---|---|---|---|
| Normal | Normal | Aneurysmal | Supracoronary tube graft | |
| Diseased | Normal | Aneurysmal | AVR + supracoronary tube graft | Wheat procedure |
| Diseased | Aneurysmal | Aneurysmal | AVR + replacement of aortic root and reimplantation of coronary arteries | Bentall |
| Normal | Aneurysmal | Aneurysmal | Valve-sparing root replacement; reimplantation of the AV into the graft | David procedure |
| Normal | Aneurysmal | Aneurysmal | Valve-sparing root replacement; remodeling of the AV into the graft via the creation of pseudo-sinuses | Yacoub procedure |
Surgery for the proximal ascending aorta, including Bentall, Wheat, David, and Yacoub procedures, is performed through a median sternotomy with CPB.
Arch Aortic Aneurysms
Surgical options for aortic arch aneurysms include hemiarch replacement, total arch replacement with or without a distal elephant trunk, and hybrid techniques that combine open surgical techniques to create endograft landing zones with TEVAR to exclude diseased aorta from circulation (Figure 9.10). A hemiarch replacement is performed in patients whose aneurysm extends to the lesser curvature of the aortic arch. In patients whose aneurysm extends to the proximal descending aorta, either a total arch replacement with reimplantation of the great vessels separately or as a button can be performed, or the elephant trunk procedure can be performed (Figure 9.10). The elephant trunk procedure includes an aortic arch graft and reimplantation of the great vessels to the prosthetic graft, in addition to either a distal 5- to 7-cm "trunk" that dangles in the proximal descending aorta (classic elephant trunk) or a distal covered stent (frozen elephant trunk; Figure 9.11). Aortic arch procedures are performed through a median sternotomy with CPB and deep hypothermic circulatory arrest (DHCA) or alternative methods that incorporate neuroprotection, which will be discussed in detail in a later section.
Figure 9.10.: Surgical Options for Thoracic Aortic Aneurysms and Dissections.
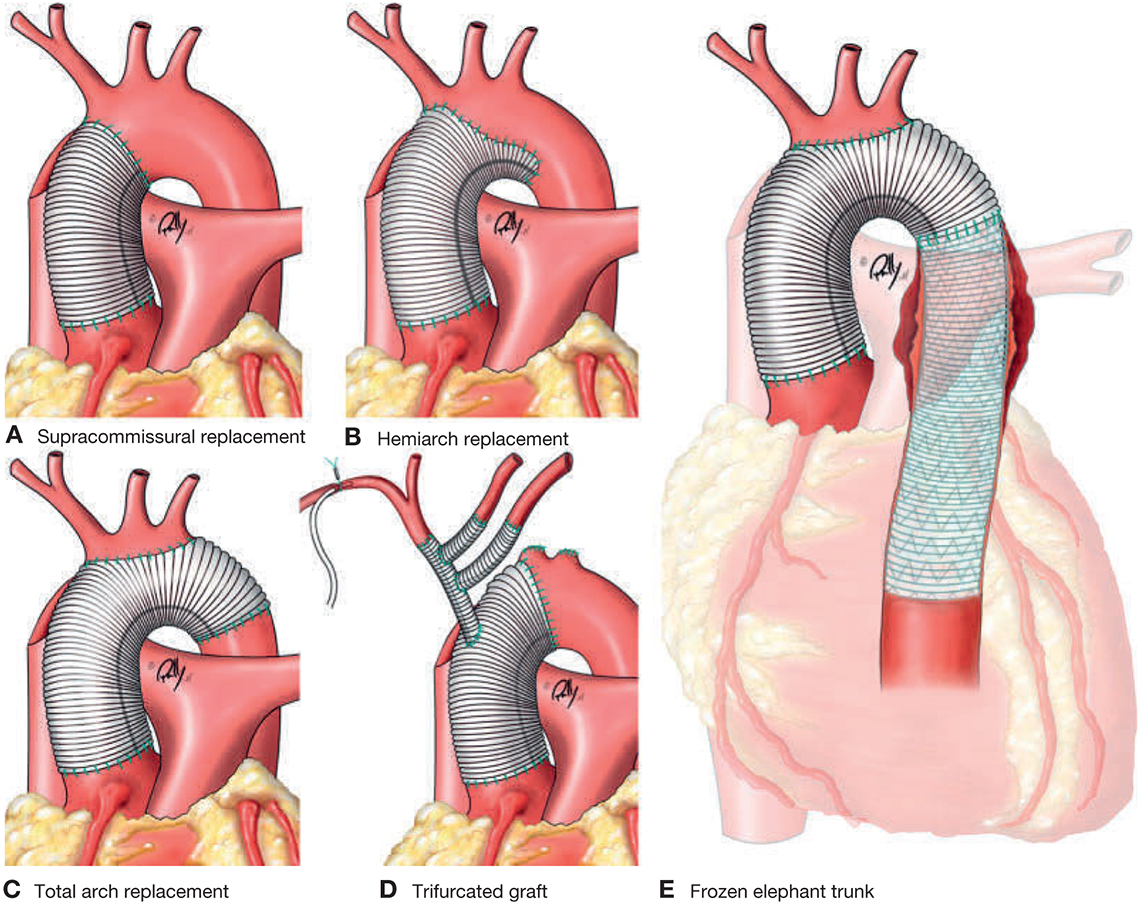
Surgical options for thoracic aortic aneurysms and dissections. A. Supracommissural replacement of the ascending aorta. B. Hemiarch replacement, aortic resection is extended to the lesser curvature (inferior portion) of the aortic arch. Reimplantation of the arch branches is not necessary. C. Total arch replacement, the aortic arch is resected, and the arch branches are reimplanted either as a button or with a composite graft. D. Trifurcated graft. E. Frozen elephant trunk (FET) procedure. (From Krüger T, Conzelmann IO, Bonser RS, et al. Acute aortic dissection type A. Br J Surg. 2012;99:1331-1344. Copyright © 2012 British Journal of Surgery Society Ltd. Reprinted by permission of John Wiley & Sons, Inc.)
Figure 9.11.: Elephant Trunk Procedure.

Elephant trunk procedure. A. Preoperative disease. B. Stage I with replacement of the ascending aorta and arch with a Dacron graft, with the distal graft sutured circumferentially to the aorta distal to the LSCA and the free end of the graft ("elephant trunk") within the descending aneurysm. C. Completion of the procedure using an endovascular stent graft attached proximally to the "elephant trunk" and the distal end secured to a Dacron graft cuff. (Reprinted from Hiratzka LF, Bakris GL, Beckman JA, et al. 2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with thoracic aortic disease. J Am Coll Cardiol. 2010;55:e27-e129.)
The hybrid approach to aortic arch aneurysm repair provides an alternative option for patients at prohibitive surgical risk for morbidity and mortality with conventional aortic arch reconstruction. A hybrid procedure creates an adequate proximal landing zone (PLZ) during open aortic reconstruction to set the stage for a distal aortic operation to be performed using a TEVAR rather than an open thoracoabdominal aneurysm repair (Figures 9.12 and 9.13). TEVAR requires planning for the proximal and distal landing zones to be at least 2 cm to ensure optimal fixation and seal. First-stage repairs can entail (1) debranching of arch vessels using a multibranched Dacron graft (type I), (2) replacement of the ascending aorta and zones 1 or 2 of the aortic arch, along with debranching of the arch vessels (type II), or (3) replacement of the ascending aorta and aortic arch with an elephant trunk (type III). Approaches to creating a PLZ without the use of sternotomy and CPB have also been described and involve the creation of a right common carotid-left common carotid-LSCA bypass (cervical arch debranching) via neck incisions.
Figure 9.12.: Surgical Strategies for Aortic Arch Debranching and Thoracic Endovascular Aortic Repair (Tevar) for Aortic Arch Aneurysms.
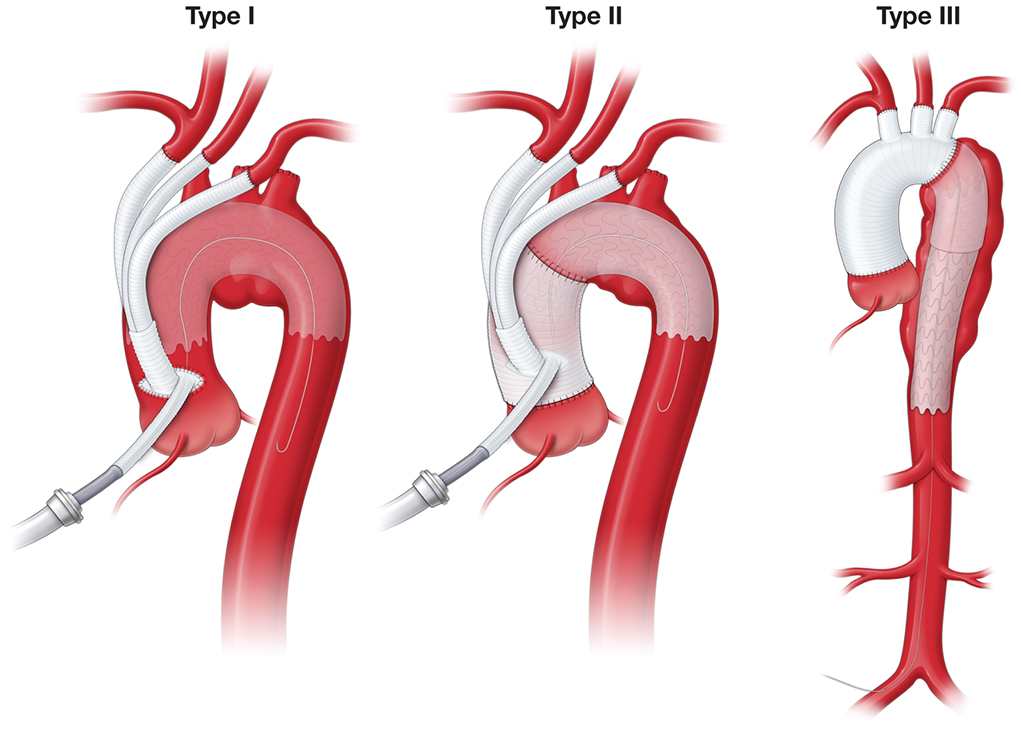
Surgical strategies for aortic arch debranching and thoracic endovascular aortic repair (TEVAR) for aortic arch aneurysms. A. Reimplantation of great vessels to the proximal ascending aorta to create a landing zone for TEVAR. B. Replacement of the ascending aorta with reimplantation of great vessels to the proximal ascending aortic graft. C. Total arch replacement, reimplantation of great vessels, and elephant trunk procedure. (Used with permission of AME Publishing Company, from Vallabhajosyula P, Szeto WY, Desai N, et al. Type II arch debranching procedure. Ann Cardiothorac Surg. 2013;2:378-386; permission conveyed through Copyright Clearance Center, Inc.)
Figure 9.13.: Illustration Demonstrating a Hybrid Aortic Arch Repair, Where an Endograft is Placed in the Aortic Arch and the Proximal Descending Aorta to Facilitate Aortic Remodeling and Create the Landing Zone for Future Reinterventions.

Illustration demonstrating a hybrid aortic arch repair, where an endograft is placed in the aortic arch and the proximal descending aorta to facilitate aortic remodeling and create the landing zone for future reinterventions. (Used with permission of AME Publishing Company, from Roselli EE. We should replace the aortic arch and more in DeBakey type I dissection—a perspective from the Cleveland Clinic. Ann Cardiothorac Surg. 2013;2:216-221; permission conveyed through Copyright Clearance Center, Inc.)
Thoracoabdominal Aneurysms
Open TAAA repair is the treatment of choice for appropriate surgical candidates but remains a challenging procedure complicated by the involvement of vital aortic branch vessels in the diseased aortic lesion. TEVAR has emerged as an alternative treatment for patients undergoing TAAA with complex aneurysms, chronic dissection, or failed aortic repair (Figure 9.14). Favorable anatomy, which includes adequate iliofemoral and brachial access, as well as suitable branch target vessels with no early bifurcation or occlusive disease, is critical for the success of the procedure. TEVARs can be performed using custom patient-specific fenestrated and branched stent grafts, though these bespoke devices are not yet readily available in many countries and cannot be utilized in more urgent clinical scenarios because they require 6 to 8 weeks to manufacture. When custom devices are not available, TEVARs can be performed with standardized multibranched stent grafts whose position is suitable for at least 50% of TAAAs treated with a patient-specific endograft; in addition, off-the-shelf devices, such as endografts with visceral parallel, that is, chimney and snorkel, grafts, can be used. Chimney/snorkel techniques involve the placement of a stent or stent graft parallel to the main aortic stent graft to extend the proximal or distal sealing zone while maintaining perfusion to the visceral and renal vessels. The concern with chimney/snorkel techniques is the potential for gutter leaks, which occur due to incomplete apposition of chimney grafts and the main body graft. It is not yet widely known whether chimney/snorkel techniques are sufficient to treat extensive TAAAs or dissections; they are also not suitable for patients with significant aortic arch atherosclerosis because they require bilateral femoral access for delivery of the main body stent and axillary/subclavian artery approaches for branch access.
Figure 9.14.: Three-Dimensional (3D) Computed Tomography Reconstruction Demonstrating Endovascular Exclusion of the Descending Thoracic Aorta Aneurysm after Abdominal and Arch Debranching.
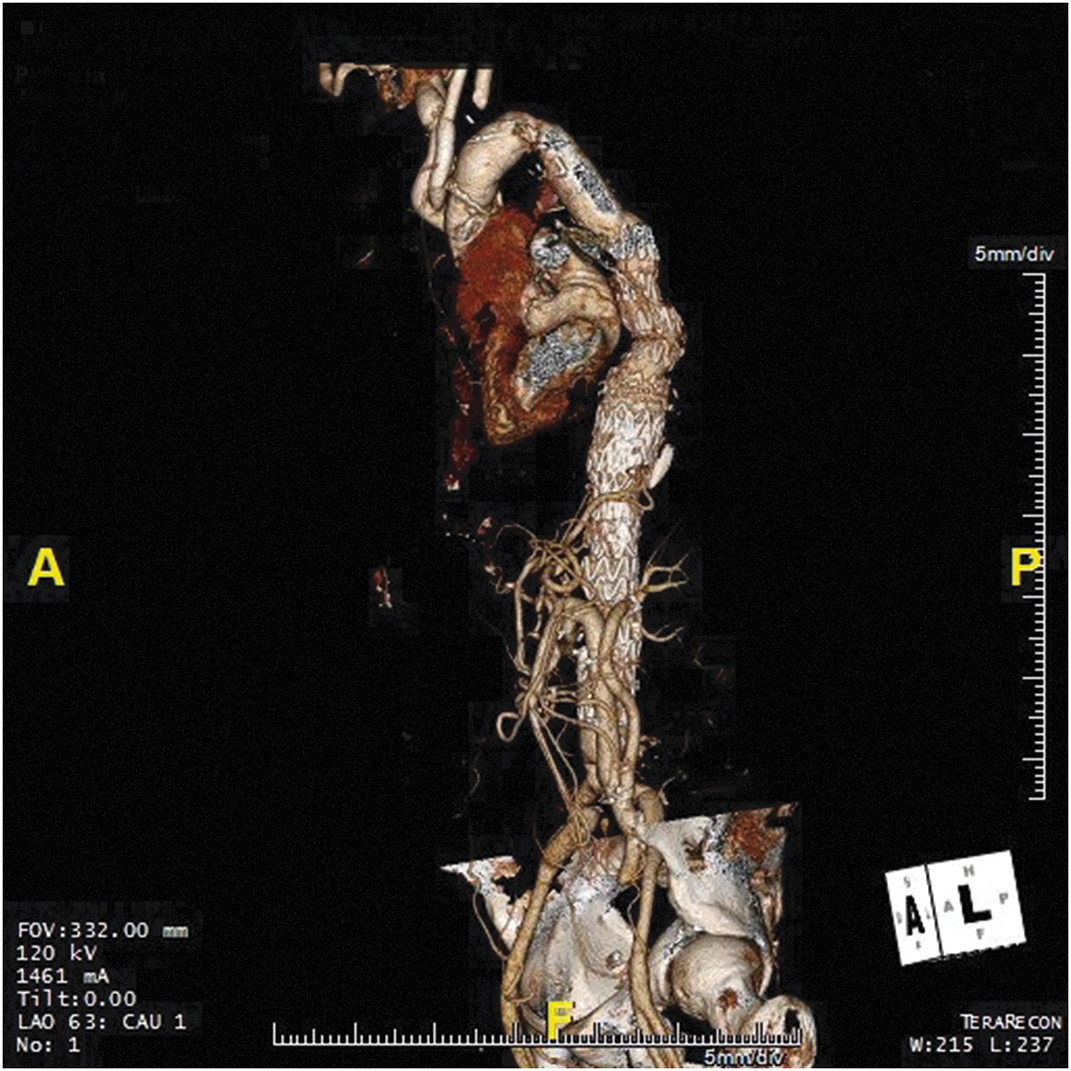
Three-dimensional (3D) computed tomography reconstruction demonstrating endovascular exclusion of the descending thoracic aorta aneurysm after abdominal and arch debranching.
Furthermore, the hybrid TAAA repair was introduced to lessen the adverse effects associated with traditional open TAAA repair through avoidance of thoracotomy, extracorporeal perfusion, single-lung ventilation, and supraceliac aortic cross-clamping, which can lead to prolonged end-organ ischemia (Figure 9.15). It also avoids the dangers of occluding vital visceral vessels. Hybrid TAAA repair starts with total abdominal debranching using retrograde extra-anatomic bypass grafts via laparotomy to reroute the visceral and renal branches from the aneurysmal segment. The debranching procedure is followed by the exclusion of the aneurysm with stent grafting. Hybrid repairs still require laparotomy and long operative times; outcomes of hybrid procedures remain controversial as they reportedly carry high 30-day mortality ranging from 10% to 26% and high complication rates for spinal cord ischemia (7%), 4.5% for mesenteric ischemia (4.5%-18%), renal failure (7%-21%), and respiratory failure (28%-30%). In lieu of debranching, a more contemporary approach involves the performance of a less extensive open Crawford extent III or IV TAAA repair to reimplant the visceral arteries onto a short section of aortic graft, followed by interval extension of the repair with a stent graft. This contemporary hybrid repair is associated with a lower risk of renal failure, spinal cord deficits, and operative mortality.
Figure 9.15.: Three-Dimensional (3D) Computed Tomography Reconstruction after Abdominal Debranching.
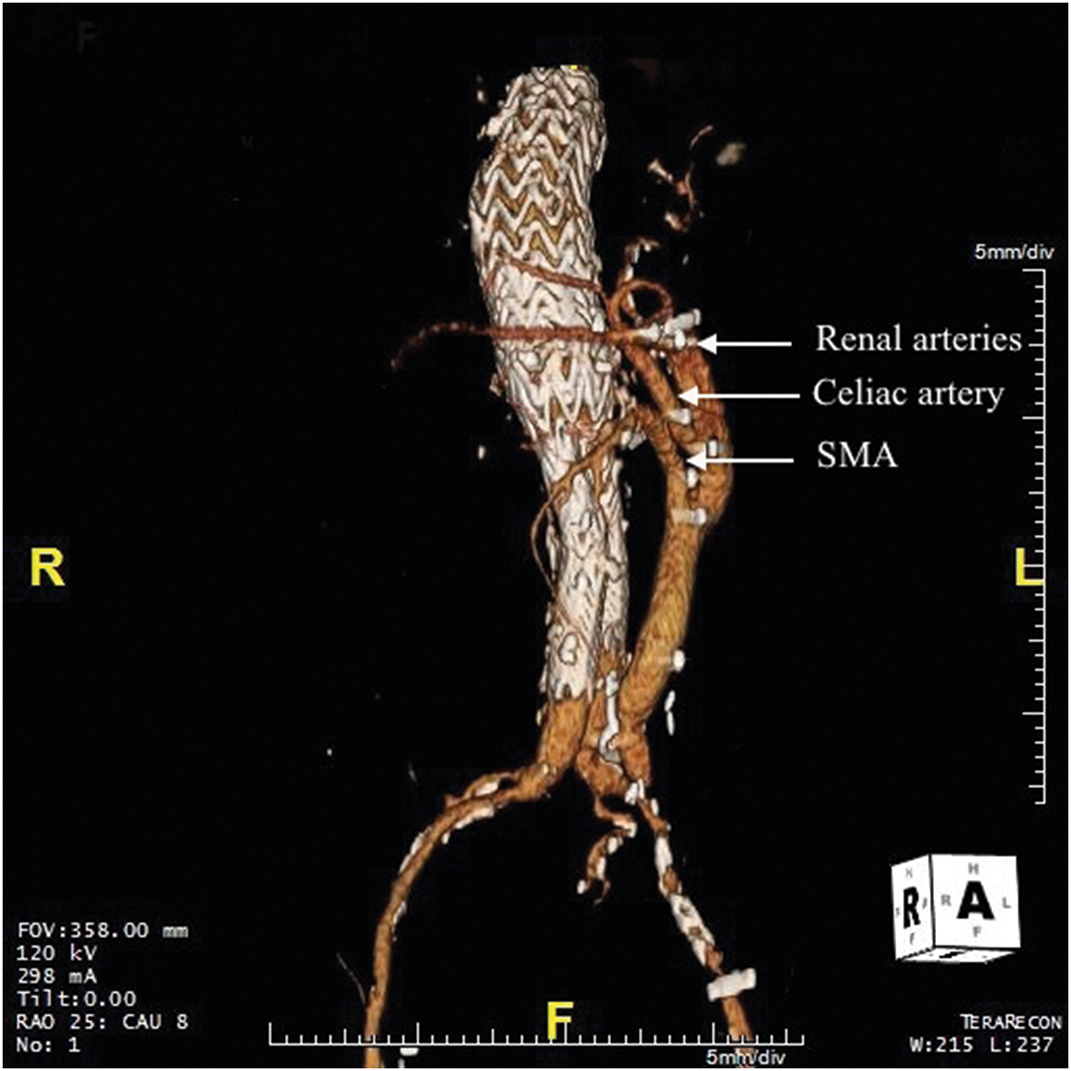
Three-dimensional (3D) computed tomography reconstruction after abdominal debranching. The superior mesenteric artery (SMA), celiac artery, and renal arteries arise from a left iliac artery graft.
References
- Bisdas T, Donas KP, Bosiers MJ, Torsello G, Austermann M. Custom-made versus off-the-shelf multibranched endografts for endovascular repair of thoracoabdominal aortic aneurysms. J Vasc Surg. 2014;60:1186-1195.
- Hughes GC, Vekstein A. Current state of hybrid solutions for aortic arch aneurysms. Ann Cardiothorac Surg. 2021;10:731-743.
- Kothari R, Weldon SA, Koksoy C, Coselli JS. Narrative review: open surgery for thoracoabdominal aortic aneurysm—is it still a horrible surgery? J Vis Surg. 2022;8:4.
- Marquis KM, Naeem M, Rajput MZ, et al. CT of postoperative repair of the ascending aorta and aortic arch. Radiographics. 2021;41:1300-1320.
- Orozco-Sevilla V, Weldon SA, Coselli JS. Hybrid thoracoabdominal aortic aneurysm repair: is the future here? J Vis Surg. 2018;4:61.
- Tanaka A, Oderich GS, Estrera AL. Total abdominal debranching hybrid thoracoabdominal aortic aneurysm repair versus chimneys and snorkels. JTCVS Tech. 2021;10:28-33.


