Objectives ⬇
- Describe the nursing informatics specialty.
- Explore the scope and standards of nursing informatics practice.
- Assess the evolving roles and competencies of nursing informatics practice.
- Appreciate the future of nursing informatics in our rich, technology-laden healthcare environments.
Key Terms ⬆ ⬇
Introduction ⬆ ⬇
In Chapter 6, History and Evolution of Nursing Informatics, you learned about the initiation of nursing informatics, how it is evolving, and the ways that all nurses use informatics in their practice. In this chapter, we will focus on nursing informatics (NI) as a specialty. NI is an established yet ever-evolving specialty. Those choosing NI as a career find it full of numerous and varied opportunities. Previously, most nurse informaticists entered the field by having an understanding of and enthusiasm for working with computers. Now, however, nurses have many educational opportunities available to become formally trained in the field of NI to become an informatics nurse specialist (INS). We will explore the scope and standards of NI; NI roles, education, and specialization; rewards of working in the field; and organizations and professional journals supporting the INS.
Nursing Contributions to Healthcare Informatics ⬆ ⬇
Nursing has been involved in the purchase, design, and implementation of information systems (ISs) since the 1970s (Saba & McCormick, 2006). One of the first health IS vendors studied how nurses managed patient care and realized that nursing activity was the core of patient activity and needed to be the foundation of the health, or clinical, IS. Nursing informaticists have been instrumental in developing, critiquing, and promoting standard nursing terminologies to be used in the health IS. Nursing is heavily involved in the design of educational materials for practicing nurses, student nurses, other healthcare workers, and patients. Computers have revolutionized the way individuals access information and educational and social networking processes.
Scope and Standards ⬆ ⬇
NI is important to nursing and health care because it focuses on representing nursing data, information, and knowledge. As identified in the 2008 edition of Nursing Informatics: Scope and Standards of Practice, NI meets the following needs for health informatics (American Nurses Association [ANA], 2008; Brennan, 1994):
- Provides a nursing perspective
- Showcases nursing values and beliefs
- Provides a foundation for nurses in NI
- Produces unique knowledge
- Distinguishes groups of practitioners
- Emphasizes the interest for nursing
- Provides needed nursing language and word context
In 2008, the ANA published a scope and standards of NI practice. This publication included the INS standards of practice and the INS standards of professional performance and addressed the who, what, when, where, how, why, and functional roles of INS practice. Three overarching standards of practice were identified (ANA, 2008):
- Incorporate theories, principles, and concepts from appropriate sciences into informatics practice.
- Integrate ergonomics and human-computer interaction (HCI) principles into informatics solution design, development, selection, implementation, and evaluation.
- Systematically determine the social, legal, and ethical impact of an informatics solution within nursing and health care. (p. 33)
In 2022, the third edition of the ANA's Nursing Informatics: Scope and Standards of Practice was released. The standards of practice and professional performance for an INS are listed in Box 7-1.
| Box 7-1 Informatics Nurse Specialist Standards of Practice and Performance |
|---|
| Standards of Professional Practice for Nursing Informatics |
|---|
- Standard 1: Assessment
- Standard 2: Diagnosis, Problems, and Issues Identification
- Standard 3: Outcomes Identification
- Standard 4: Planning
- Standard 5: Implementation
- Standard 5A: Coordination of Activities
- Standard 5B: Health Teaching and Health Promotion
- Standard 6: Evaluation
|
| Standards of Professional Performance for Nursing Informatics |
|---|
- Standard 7: Ethics
- Standard 8: Culturally Congruent Practice
- Standard 9: Communication
- Standard 10: Collaboration
- Standard 11: Leadership
- Standard 12: Education
- Standard 13: Evidence Based Practice and Research
- Standard 14: Quality of Practice
- Standard 15: Professional Practice Evaluation
- Standard 16: Resource Utilization
- Standard 17: Environmental Health
Data from: American Nurses Association. (2022). Nursing informatics: Scope and standards of practice (2nd ed.). Nursesbooks.org. |
The ANA (2018) also described the major functional areas of nursing informatics as follows:
- Administration, leadership, and management
- Analysis
- Compliance and integrity management
- Consultation
- Coordination, facilitation, and integration
- Development
- Education and professional development
- Policy development and advocacy
- Research and evaluation (para. 6)
As INSs assume their roles, it is evident that typical roles cover more than one functional area and that their “informatics solutions are more closely integrated with the delivery of care” (ANA, 2015, p. 36). The ANA also denoted telehealth as an integrated functional area that is a dynamic health information technology. As nursing, information, computer, and cognitive sciences continue to evolve, so will NI functions. For example, Kim (2020) pointed out the growing need for INSs to be fully aware of cybersecurity threats and prepared to act in cases of intentional tampering with patient information systems. According to the ANA (2018), “informatics nurses of all levels practice at the intersection of technology and clinical practice” (para. 7). With the rapid advancements we have already seen in the previous decade, we know that the INSs of the future will be assuming roles and working in areas that we have not yet imagined.
Nursing Informatics Roles ⬆ ⬇
NI has become a viable and essential nursing specialty with the introduction of computers, technology, and the electronic health record (EHR) to health care. Many nurses entered the NI field because of their natural curiosity and dedication to being lifelong learners. Others who entered this field might have done so by accident. Perhaps they were comfortable working with computers, and their coworkers used them as a resource for computer-related questions. The introduction of the EHR has forced all clinicians to learn to use this new technology and incorporate it into their already busy days. According to Baumann et al. (2018), who conducted a systematic review and meta-analysis, nursing documentation time increased from 9% before EHR to 23% after EHR implementation. Assisting nurses to incorporate this new technology into their daily workflow is one of many challenges that the INS may tackle. Even though INSs appear to work behind the scenes, they affect the health and clinical outcomes of patients.
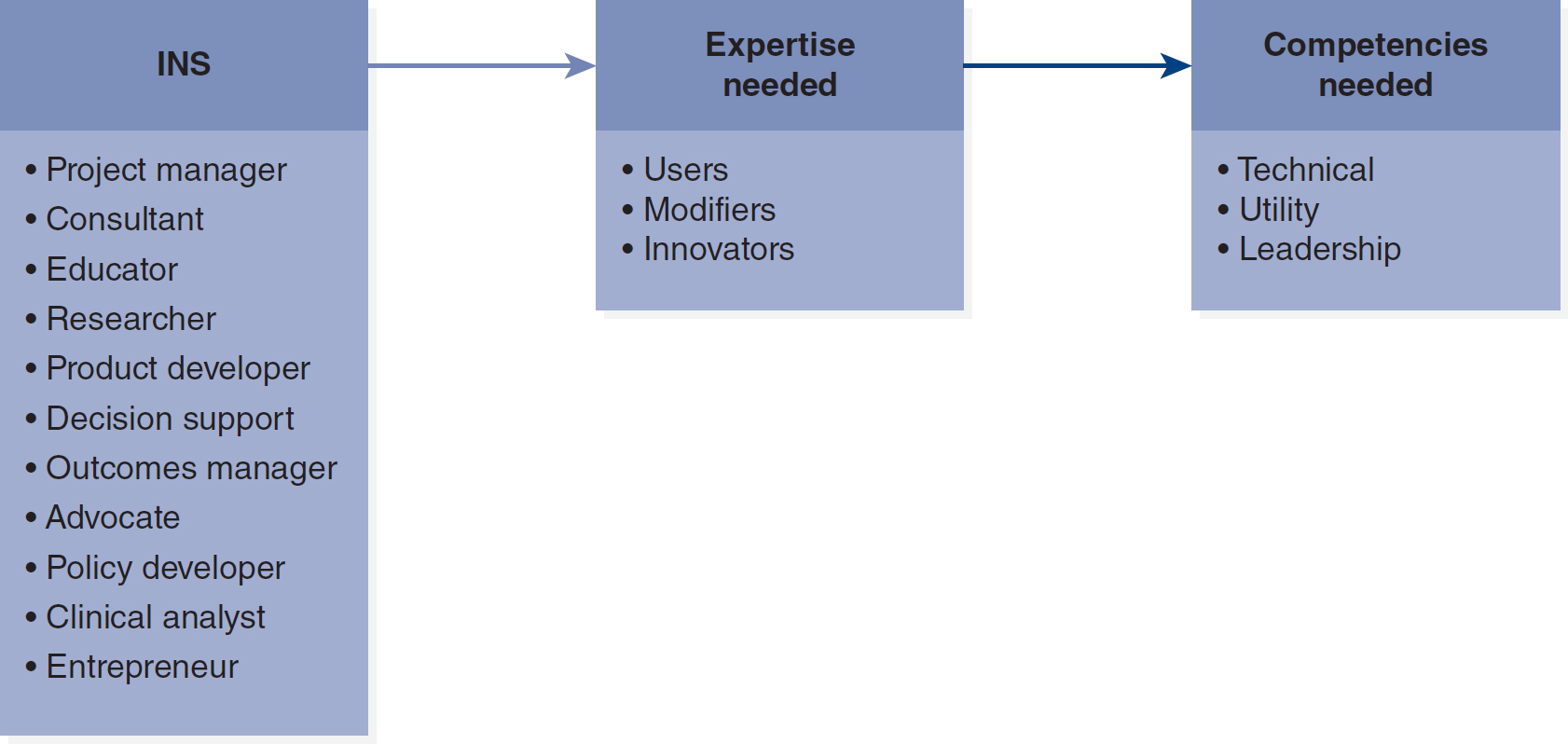
The INS may take on numerous roles (Figure 7-1). For example, one position that INSs fill quite well is the role of project manager as a result of their ability to simultaneously manage multiple complex situations. Because of the breadth of the NI field, however, many INSs find that they need to further specialize. The following list includes some typical INS positions, though it is far from comprehensive because this field changes rapidly, as does technology (ANA, 2015, 2022; Thede, 2003).
Figure 7-1 Nursing Informatics Roles
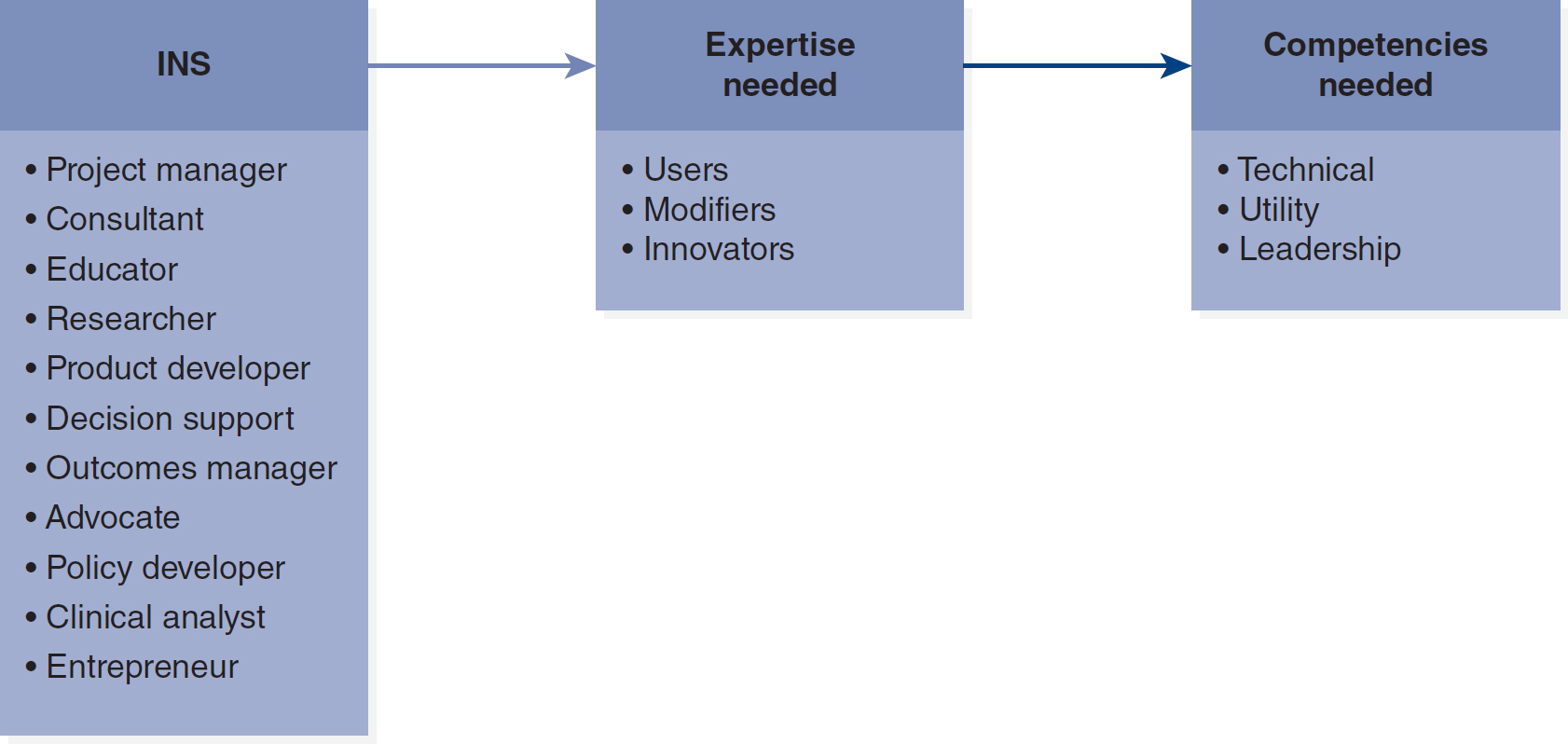
A flow diagram depicts various roles in nursing informatics.
The key roles include Informatics Nurse Specialist, I N S, functioning as a project manager, consultant, educator, researcher, product developer, decision support, outcomes manager, advocate, policy developer, clinical analyst, and entrepreneur. Expertise needed spans users, modifiers, and innovators. Competencies needed encompass technical, utility, and leadership skills.
- Project manager: In the project manager role, the INS is responsible for the planning and implementation of informatics projects. The INS uses the skills of communication, change management, process analysis, risk assessment, scope definition, and team building. This role acts as the liaison among clinicians, management, IS personnel, stakeholders, vendors, and all other interested parties.
- Consultant: The INS who takes on the consultant role provides expert advice, opinions, and recommendations based on their area of expertise. Flexibility, good communication skills, excellent interpersonal skills, and extensive clinical and informatics knowledge are highly desirable skill sets that the NI consultant needs.
- Educator: The success or failure of an informatics solution can be directly related to the education and training that are provided for end users. The INS who chooses the educator role develops and implements educational materials and sessions and provides education about the system to new or current employees during a system implementation or an upgrade.
- Researcher: The researcher role entails conducting research (especially data mining) to create new informatics and clinical knowledge. Research may range from basic informatics research to developing clinical decision support tools for nurses.
- Product developer: An INS in the product developer role participates in the design, production, and marketing of new informatics solutions. An understanding of business and nursing is essential in this role.
- Decision support/outcomes manager: Nurses assuming the role of decision support/outcomes manager use tools to maintain data integrity and reliability. Contributing to the development of a nursing knowledge base is an integral component of this role.
- Advocate/policy developer: INSs are key to advocating for the patients and healthcare systems and developing the infrastructure of health policy. Policy development on local, national, and international levels is an integral part of the advocate/policy developer role.
- Clinical analyst/systems specialist: INSs may work at varying levels and serve as a link between nursing and information services in healthcare organizations.
- Entrepreneur: The nurses involved in the entrepreneur role combine their passion, skills, and knowledge to develop marketable business ideas by analyzing nursing information needs and developing and marketing solutions.
The Nursing Informatics Working Group of the American Medical Informatics Association (AMIA; n.d.) identified the following core responsibilities for nurse informaticists to embrace:
- Concept representation and standards to support evidence-based practice, research, and education
- Data and communication standards to build an interoperable national data infrastructure
- Research methodologies to disseminate new knowledge into practice
- Information presentation and retrieval approaches to support safe patient centered care
- Information and communication technologies to address inter-professional workflow needs across all care venues
- Vision and management for the development, design, and implementation of communication and information technology
- Definition of healthcare policy to advance the public's health (para. 3)
These expanded responsibilities make clear that nurse informaticists will be instrumental in knowledge building and dissemination, promoting interoperability, supporting safe patient-centered care, ensuring interprofessional workflow and communications, and participating in key health policy decisions.
Specialty Education and Certification ⬆ ⬇
Many of the original nurses who entered into NI did so without any formal education in this field. In many cases, these nurses served as the unit resource for computer or programming questions. Often, they acquired their skills through on-the-job training or by attending classes. Although this pathway to the NI field is still available today, more formal ways of acquiring these skills exist. The informatics nurse has a Bachelor of Science degree in nursing and additional knowledge and expertise in the informatics field (ANA, 2022). The INS holds an advanced degree or a post-master's certificate and is prepared to assume roles requiring this advanced knowledge. INSs may attend informatics conferences and obtain contact hours or continuing education units.
Box 7-2 lists some of the pioneering colleges and universities that offer advanced degrees or certificates in NI. This is not a comprehensive list because new programs are continually being developed. You should research local colleges and universities to see which ones have informatics programs.
| Box 7-2 Formal Nursing Informatics Educational Programs |
|---|
| Graduate Degree Programs |
|---|
|
| Certificate Programs |
|---|
|
It is important to distinguish between earning a certificate in nursing informatics and earning certification. As provided in Box 7-2, there are several certificate (educational) programs in nursing and/or health informatics. A certificate program “is an educational or training program that is used to teach learning objectives and assess whether those objectives were achieved by the student” (Institute for Credentialing Excellence, n.d., para. 2). In contrast, certification is a program “designed to test the knowledge, skills, and abilities required to perform a particular job, and, upon successfully passing a certification exam, to represent a declaration of a particular individual's professional competence” (para. 2).
Nurses who choose to specialize in informatics have several certification options available to them. The only certification specific to nursing informatics is offered through the American Nurses Credentialing Center, and the successful candidate is identified by the RN-BC credential. The applicant must be a licensed registered nurse with at least 2 years of recent experience and have a baccalaureate degree in nursing or a related field. The applicant must have completed 30 contact hours of continuing education in informatics within the past 3 years. The applicant must meet one of the following criteria for practice hours: (1) 2,000 hours practicing as an informatics nurse in the past 3 years, (2) 1,000 hours practicing as an informatics nurse and 12 semester hours of graduate academic credit toward an NI degree, or (3) completion of an NI degree that included at least 200 supervised practicum hours. For further information on this certification examination, visit www.nursingworld.org/our-certifications/informatics-nurse. This website includes the aforementioned criteria and provides further information about test eligibility, fees, examination content and locations, study materials, and practice tests.
The Healthcare Information and Management Systems Society (HIMSS) sponsors two certification examinations-Certified Associate in Healthcare Information and Management Systems (CAHIMS) and Certified Professional in Healthcare Information and Management Systems (CPHIMS). Candidates who successfully pass the CPHIMS examination are designated as certified professionals in healthcare information and management systems. The HIMSS examinations are open to any candidate who is involved in healthcare informatics. For CPHIMS certification, candidates must hold a position in one of the following fields: administration/management, clinical IS, eHealth, IS, or management engineering. Candidates may include any of the following roles: chief executive officers, chief information officers, chief operating officers, senior executives, senior managers, IS technical staff, physicians, nurses, consultants, attorneys, financial advisers, technology vendors, academicians, management engineers, and students. For more information on the HIMSS certification processes, please visit www.himss.org/resources/certification.
Mack (n.d.) provided an overview of additional certifications that are available or in development in healthcare informatics: Registered Health Information Administrator (RHIA) certification, offered by the American Health Information Management Association (AHIMA) (www.ahima.org/certification-careers/certifications/rhia), and AMIA Health Informatics Certification (AHIC), through AMIA (https://amia.org/ahic).
Nursing Informatics Competencies ⬆ ⬇
An ongoing challenge that has been identified in the literature and that will likely continue to plague health care is the vast differences in computer literacy and information management skills that healthcare workers possess (Gassert, 2008; McNeil et al., 2006; Topkaya & Kaya, 2015).
As early as 2001, Staggers et al. advocated that nursing students and practicing nurses should be educated on core NI competencies. Although information technology (IT) and informatics concepts certainly need to be incorporated into nursing school curricula, progress in this area has been slow. In the 1980s, a nursing group of the International Medical Informatics Association convened to develop the first level of nursing competencies. While developing these competencies, the nursing group found that nurses fell into one of the following three categories: (1) user, (2) developer, or (3) expert. These categories have since been expanded.
Staggers and colleagues (2001) decided that the NI competencies that were developed in the 1980s were inadequate and needed to be updated. These authors reviewed 35 NI competency articles and 14 job descriptions, which resulted in 1,159 items that were sorted into three broad categories: (1) computer skills, (2) informatics knowledge, and (3) informatics skills. These items were then placed in a database, where redundant items were removed. When this process was completed, 313 items remained.
When these items were then further subdivided, Staggers and colleagues (2001), along with the AMIA work group, realized that these competencies were not universal to all nurses; thus, before they could determine whether the competency was an NI competency, the nursing skill levels needed to be defined. The group determined that practicing nurses could be classified into four categories: (1) beginning nurse, (2) experienced nurse, (3) INS, and (4) informatics innovator. Each of these skill levels needed to be defined before Staggers and colleagues could determine which level was the most appropriate for that skill set.
Staggers et al. (2002) conducted the seminal work in this area, a Delphi study to validate the placement of the competencies into the correct skill level. Of the 305 original competencies identified, 281 achieved an 80% approval rating for both importance as a competency and placement in the correct practice level. The authors stressed that this is a comprehensive list; thus, for a nurse to enter a particular skill level, they need not have mastered every item listed for that skill level. For a list of competencies identified by nursing skill level, see Table 7-1.
Table 7-1 Nursing Informatics Competencies by Skill LevelBased on research conducted by Hunter et al. (2013), the online TIGER-based self-assessment instrument, Assessment of Nursing Informatics Competencies (TANIC), was developed. This instrument assesses the Level 1: Beginning Nurse and Level 2: Experienced Nurse competencies. |
Level 1: Beginning Nurse |
- Start the computer and log on securely to access select applications/software
|
|
- Collect and enter patient data into the information system
|
Level 2: Experienced Nurse |
- Identify the risks and limitations of surfing the internet to locate evidence-based practice information
|
- Gather data to draw and synthesize conclusions
|
- Explain how to sustain the integrity of information resources
|
Based on the research conducted by McGonigle et al. (2015), the online self-assessment instrument, Nursing Informatics Competency Assessment-Level 3/Level 4 (NICA L3/L4), was developed. This instrument assesses the Level 3: Informatics Nurse Specialist and Level 4: Informatics Innovator competencies. |
Level 3: Informatics Nurse Specialist |
- Fluent in nursing informatics and nursing terminologies
|
- Apply aspects of human technology interface to screen, device, and software design
|
- Teach nurses how to locate, access, retrieve, and evaluate information
|
Level 4: Informatics Innovator |
|
- Transform software programs to support data analysis and aggregation
|
- Lead research efforts to determine and address application needs
|
Hunter, K. M., McGonigle, D., & Hebda, T. (2012, June 23-27). Operationalizing TIGER NI competencies for online assessment of perceived competency. 11th International Congress on Nursing Informatics, Montreal, Canada, 181.
In 2004, a group of nurses came together after attending a national informatics conference to ensure that nursing was equally recognized in the national informatics movement. This so-called Technology Informatics Guiding Education Reform (TIGER) team determined that using informatics was a core competency for all healthcare workers. They also determined that many nurses lacked IT skills, which limited their ability to access evidence-based information that could otherwise be incorporated into their daily practice. This group developed a plan to include informatics courses in all levels of nursing education (HIMSS, n.d.-b). Many of the items identified by the TIGER team as lacking in both nursing students and practicing nurses are ones that Staggers et al. (2002) determined to be NI competencies. To learn more about the TIGER initiative, visit www.himss.org/professionaldevelopment/tiger-initiative.
Through the work of Hunter et al. (2012, 2013, 2015) and McGonigle et al. (2013, 2015), the competencies for nursing informatics practice levels 1 through 4 have been further refined with two self-assessment tools that have been developed. Hunter and colleagues focused on the level 1 and level 2 competencies and developed the self-assessment of competencies TANIC tool, TIGER-Based Assessment of Nursing Informatics Competencies. McGonigle and colleagues focused on the competencies related to the advanced levels 3 and 4 and developed the self-assessment of competencies NICA L3/L4 tool, Nursing Informatics Competency Assessment Level 3/Level 4. “Together, these two instruments allow for comprehensive assessment of informatics competencies and hold international recognition” (ANA, 2022, p. 63).
It is critical for nurses and INSs to demonstrate competence. Because there were many definitions of the term competency, the authors of these tools had to first define the term. Hunter et al. (2013) concluded the following:
Competency, then, is a concept applicable to multiple situations. At its most basic, competency denotes having the knowledge, skills, and ability to perform or do a specific task, act, or job. Depending on the context, competency can refer to adequate or expert performance. For this research, competency was used to mean adequate knowledge, skills, and ability. Nursing-informatics competency was defined as adequate knowledge, skills, and ability to perform specific informatics tasks. (p. 71)
The teams began instrument development by synthesizing both seminal and current literature to construct instrument items; they reviewed, formatted, and initiated instrument testing with a Delphi study and then piloted the resulting instrument with experts. Cronbach's alpha values were calculated. The TANIC Cronbach was 0.944 for clinical information management, 0.948 for computer skills, and 0.980 for information literacy. The NICA L3/L4 reliability estimates were as follows: computer skills, 0.909; informatics knowledge, 0.982; and informatics skills, 0.992. The Cronbach's reliability estimates for each tool showed strong internal consistency reliability.
The TANIC self-assessment instrument included questions about demographics and the self-assessment, consisting of 85 items that cover basic computer literacy, clinical information management, and information literacy. The NICA L3/L4 self-assessment instrument included questions about demographics and the 178-item self-assessment, consisting of computer skills, informatics knowledge, and informatics skills.
These tools and those that will follow are extremely important because they help each of us identify our own level of comfort with technology and our self-confidence in our ability to perform these skills and tasks. Nurse educators in all practice settings and school-based programs must help their nurses or nursing students recognize deficits in their current knowledge and skills. The nurse educators can facilitate the professional development of their nurses or nursing students through the identification of courses or skill-based labs that will help them turn their deficits into strengths.
Value and Rewards of Nursing Informatics Practice ⬆ ⬇
NI is a nursing specialty that does not focus on direct patient care but instead focuses on enhancing patient care and safety and improving the workflow and work processes of nurses and other healthcare workers. The INS is instrumental in designing the EHRs that healthcare workers use on a daily basis. This nurse is also responsible for designing tools that allow healthcare workers to access patient information more efficiently than they have been able to do in the past. The ANA (2022) pointed out that informatics nurses (INs) and INSs possess a “unique contextual understanding of the healthcare ecosystem” (p. 6). The INS brings value to an organization because of specialized practice expertise and a unique understanding of organizations, health policy, and research.
Change is a factor that an INS deals with daily. The dynamic nature of this position is probably its most difficult aspect because people deal with change differently. Understanding change theory and processes and appreciating how change affects people assist the INS in developing strategies to encourage healthcare workers to accept changes and become proficient in informatics solutions that have been implemented. Seeing the change adopted with a minimal amount of discord is very rewarding to the INS.
INSs also participate in informatics organizations that allow them to network and share experiences with one another. Such interactions allow them to bring new solutions back to their respective organizations and improve informatics trouble spots. Attending professional conferences allows INSs to stay abreast of changes in the industry. Continuing education may help INSs to improve a process or workflow within the hospital or to change the way a system upgrade is implemented.
Nursing Informatics Organizations and Journals ⬆ ⬇
One of the first informatics organizations founded was HIMSS. Launched in 1961, HIMSS celebrated its 62nd year in 2023 and now has offices throughout the United States and Europe. HIMSS currently represents more than 120,000 individuals and 650 corporations; supports both local and national chapters; and has many associated work groups, one of which is an NI work group. HIMSS is well known for its development of industry-wide policies and its educational and professional development initiatives, all of which are directed toward the goal of ensuring safe patient care. Membership in HIMSS offers many advantages for nurses, such as access to numerous weekly and monthly publications and a scholarly journal, the Online Journal of Nursing Informatics. HIMSS offers several educational programs, including virtual expos, which allow participants to experience the expo without having to travel. These educational opportunities allow participants to network with colleagues and peers, which is a valuable asset in this field. HIMSS also periodically conducts NI workforce surveys. It is interesting to review the most current survey results and compare them to your setting and role.
The AMIA was founded in 1990 when three health informatics associations merged. It currently has more than 3,000 members who reside in 42 countries. Its focus is on the development and application of biomedical and healthcare informatics. Members include physicians, nurses, dentists, pharmacists, health IT professionals, and biomedical engineers. AMIA offers many benefits to its members, such as weekly and monthly publications and a scholarly journal, JAMIA: Journal of the American Medical Informatics Association. Members may join a working group that is specific to their specialty, including an NI working group. AMIA offers multiple opportunities for educational and networking pursuits.
The American Nursing Informatics Association (ANIA) was established in 1992 to provide an opportunity for Southern California informatics nurses to meet. It has since grown into a national organization whose members include healthcare professionals who work with clinical ISs, educational applications, data collection/research applications, and administrative/decision support systems (DSSs) as well as those who have an interest in the field of NI. In 2009, ANIA merged with the Capital Area Roundtable on Informatics in Nursing. Membership benefits include the following:
- Access to a network of more than 3,200 informatics professionals in 50 states and 30 countries
- Active email list
- Quarterly newsletter indexed in CINAHL and Thomson
- Job bank with employee-paid postings
- Reduced rate at the ANIA Annual Conference
- Reduced rate for CIN: Computers, Informatics, Nursing
- ANIA Online Library of on-demand and webinar education activities
- Membership in the Alliance for Nursing Informatics
- Web-based meetings
- In-person meetings and conferences held nationally and worldwide
The Alliance for Nursing Informatics (ANI) is a coalition of NI groups that represents more than 3,000 nurses and 20 distinct NI groups in the United States. Its membership represents local, national, and international NI members and groups. These individual groups have developed organizational structures and established programs and publications. ANI functions as the link between NI organizations and the general nursing and healthcare communities and serves as the united voice of NI.
Box 7-3 lists some of the organizations that have been instrumental in establishing the informatics community along with their publications, but many other informatics groups exist.
| Box 7-3 Nursing Informatics Websites and Corresponding Journals |
|---|
- Alliance for Nursing Informatics
- American Health Information Management Association
- Website: www.ahima.org
- Journal: Journal of AHIMA and Perspectives in Health Information Management (online)
- American Medical Informatics Association
- American Nursing Informatics Association
- Website: www.ania.org (includes Capital Area Roundtable on Informatics in Nursing)
- Journal: Journal of Informatics Nursing
- Health Information and Management Systems Society
- International Medical Informatics Association
|
The Future of Nursing Informatics ⬆ ⬇
NI is still in its infancy, as is the technology that the INS uses on a daily basis. NI will continue to influence the development of interoperable EHRs to accurately capture and share patient data and capture the care that nurses give to patients. These are formidable challenges because much of the care provided by nurses is intangible in nature and we are still struggling with EHRs that can seamlessly share health information. In the future, the EHR will provide data to the INS that can be analyzed and then used to improve nursing workflow and determine whether current practices are the most efficient and beneficial to the patient. The HIMSS 2017 Nursing Informatics Workforce Survey reported that the most frequent job responsibilities of the INS are systems implementation, systems optimization/utilization, systems development, clinical analytics, quality initiatives and reporting, informatics education, liaison/communicator, and regulatory initiatives. The HIMSS 2020 Nursing Informatics Workforce Survey reported that the job responsibilities had remained consistent with those identified in the 2017 survey; however, project management and change control/management surfaced as new responsibilities. Nursing and health care are on a roller-coaster ride that will undoubtedly prove very interesting. New technology is being introduced at a breakneck speed, and nursing and health care must be ready to ride this roller coaster. Programs need to be developed to keep nurses and healthcare workers abreast of the technological changes as they occur, and educating new and current nurses presents a significant challenge to the INS. Therefore, the INS's future looks very promising and rewarding, and demand for INSs is only expected to grow.
As the future becomes yesterday, people are waking up to the fact that we need the entire healthcare team prepared with informatics competencies. All healthcare providers should receive education on informatics because they need basic informatics skills, such as the ability to use search engines to find information about a specific topic. Consequently, all healthcare providers must attend classes to improve their computer skills and knowledge, and those entering the nursing field need a general knowledge of computer capabilities. Many new trends-such as Web 2.0, increased attention to evidence-based practice, and a better understanding of genomics-will affect care delivery in the 21st century, and NI nurses must be prepared to lead these efforts to improve care and help nurses have a voice in the informatics skills they need and the advances and tools they use, including the EHR (Bakken et al., 2008; Lavin et al., 2015).
INSs are also in a unique position to lead interprofessional team collaboration efforts. An interprofessional team is a collection of professionals (e.g., physicians, nurses, pharmacists, physical therapists, and nutritionists) who work together to deliver patient care and improve outcomes. Although the EHR is the primary documentation tool for professionals, sometimes it is difficult to surface important care information and viewpoints of other professionals because finding the documentation of other professionals may not be intuitive. INSs educated in a collaborative practice philosophy understand how to reach across professional boundaries and surface and support the unique contributions of professionals to patient care. As Christopherson et al. (2015) pointed out, “Integrated competency is essential for eliminating information silos, duplication and redundancy. Effective utilization of and implementation of technology is dependent on clinical tools that are intentionally designed to support and enhance the scopes of practice of the interprofessional team members” (p. 12). The INS is uniquely positioned to ensure that the IT tools are used effectively. Similarly, Holden et al. (2018) advocated for the involvement of informatics professionals in interprofessional team collaboration efforts. They identified seven best practices for informaticians to support interprofessional collaboration:
- Adopt the characteristics of effective teams.
- Practice leadership and followership.
- Clearly communicate with the aid of tools.
- Design team meetings for effectiveness and efficiency.
- Articulate your skills with respect to health informatics.
- Develop skills and knowledge in interprofessional teamwork and domains.
- Ensure health informatics education supports interprofessional collaboration. (p. 143)
Change plays a significant part in health care today, and those interested in NI must embrace change. They must also be good at enticing others to embrace change if they want to truly transform healthcare practices and ensure excellent outcomes. Nevertheless, NI candidates must realize that change is often accompanied by resistance. For their part, INSs must be ready to leave the bedside because nurses entering into this field will no longer be giving hands-on care. NI is a very challenging but rewarding field. In an ideal world, all healthcare agencies would employ at least one INS, and all nurses would embrace the knowledge worker title.
We would be remiss if we did not acknowledge NI and health technology initiatives worldwide. We tend to be ethnocentric in our belief that the United States is the only leader in informatics when in fact there are strong informatics initiatives in many other countries. Cummins et al. (2016) identified nursing informatics societies in eight other countries: Australia, Canada, England, Ireland, Korea, New Zealand, Singapore, and Taiwan. In 2020, the 15th International Congress on Nursing Informatics was held in Brisbane, Australia. Previous international conferences were held in Mexico (2018), Switzerland (2016), Taiwan (2013), Canada (2012), Finland (2009), and Korea (2006). The HIMSS (n.d.-a) indicates that there are 58 chapters in the United States, Canada, and India.
In 2014, the Centers for Disease Control and Prevention (CDC; n.d.) launched a Global Health Security Agenda (GHSA) with the goal of quickly identifying and containing public health threats. We will learn more about CDC initiatives in Chapter 17, Using Informatics to Promote Community and Population Health. It is clear that the reach of informatics and health technology is worldwide and ever expanding.
Summary ⬆ ⬇
According to the ANA (2022), “NI is the specialty that transforms data into needed information and leverages technologies to improve health and health care equity, safety, quality, and outcomes” (p. 6). Here is our expanded definition of NI: the synthesis of nursing science, information science, computer science, and cognitive science for the purpose of managing, disseminating, and enhancing healthcare data, information, knowledge, and wisdom to improve collaboration and decision-making; provide high-quality patient care; and advance the profession of nursing. Informatics practices support nurses as they seek to care for their patients effectively and safely by making the information that they need more readily available. Nurses have been actively involved in this field since computers were introduced to health care. With the advent of the EHR, it became apparent that nursing needed to develop its own terminology related to the new technology and its applications; NI has been instrumental in this process.
Today, the healthcare industry employs the largest number of knowledge workers in the world. Nurses, as knowledge workers in technology-laden healthcare facilities, must continually improve their informatics competencies. The INS is instrumental in leading the advancement of informatics concepts and tools in all settings and across all specialties. NI is a specialty governed by standards that have been established by the ANA. Because NI is a very diverse field, many INSs eventually specialize in one segment of the field. Although NI is an established specialty, all nurses utilize the core NI principles. Nursing informatics competencies have been developed to encompass all levels of practice and ensure that entry-level nurses are ready to enter the more technologically advanced field of nursing as well as establishing advanced competencies for the INS's specialty practice. These competencies may be used to determine the educational needs of current staff members.
The growth of the NI field has resulted in the formation of numerous NI organizations or nursing subgroups of the medical informatics organizations. Nurses no longer have to enter the field by chance but instead can obtain an advanced degree in NI at many well-established universities. In addition, INSs may continue their learning by attending the numerous conferences offered.
NI has grown tremendously as a specialty since its inception and is expected to continue to grow. The NI specialty not only engages nurses and patients but also engages data to improve patient outcomes, enhance patient care, and advance the science of nursing. It will be interesting to see where NI and INSs take health care in the future.
| Thought-Provoking Questions |
|---|
- A hospital is seeking to update its EHRs. It has been suggested that an INS be hired. This position does not involve direct patient care, and the administration is struggling with how to justify the position. How can this position be justified?
- It is important that all nurses be informatics competent at all levels. In particular, at which levels should the INS be able to exhibit competency? Provide several examples of the knowledge and skills that an INS might demonstrate.
- How does nursing move from measuring the tasks completed to measuring the final outcome of the patient? How can the INS help us reach this goal?
|
References ⬆
- American Medical Informatics Association. (n.d.). Nursing informatics. www.amia.org/programs/working-groups/nursing-informatics
- American Nurses Association. (2008). Nursing informatics: Scope and standard of practice. Nursesbooks.org.
- American Nurses Association. (2015). Nursing informatics: Scope and standard of practice (2nd ed.). Nursesbooks.org.
- American Nurses Association. (2018). Nursing informatics: The intersection of technology and clinical practice. www.wolterskluwer.com/en/expert-insights/nursing-informatics-the-intersection-of-technology-and-clinical-practice
- American Nurses Association. (2022). Nursing informatics: Scope and standard of practice (3rd ed.). Nursesbooks.org.
- Bakken S., Stone P., & Larson E. (2008). A nursing informatics research agenda for 2008-18: Contextual influences and key components. Nursing Outlook, 56(5), 206-214. https://doi.org/10.1016/j.outlook.2008.06.007
- Baumann L. A., Baker J., & Elshaug A. G. (2018). The impact of electronic health record systems on clinical documentation times: A systematic review. Health Policy, 122(8), 827-836. https://doi.org/10.1016/j.healthpol.2018.05.014
- Brennan P. F. (1994). On the relevance of discipline to informatics. Journal of the American Medical Informatics Association, 1(2), 200-201. https://doi.org/10.1136/jamia.1994.95236150
- Centers for Disease Control and Prevention. (n.d.). Global health protection and security. www.cdc.gov/globalhealth/healthprotection/about.html
- Christopherson T. A., Troseth M. R., & Clingerman E. M. (2015). Informatics-enabled interprofessional education and collaborative practice: A framework-driven approach. Journal of Interprofessional Education & Practice, 1(1), 10-15. https://doi.org/10.1016/j.xjep.2015.03.002
- Cummins M. R., Gundlapalli A. V., Murray P., Park, H.-A., & Lehmann C. U. (2016). Nursing informatics certification worldwide: History, pathway, roles, and motivation. Yearbook of Medical Informatics, 25(1), 264-271. https://dx.doi.org/10.15265/IY-2016-039
- Gassert C. (2008). Technology and informatics competencies. Nursing Clinics of North America, 43(4), 507-521. https://doi.org/10.1016/j.cnur.2008.06.005
- Health Information and Management Systems Society. (n.d.-a). Member participation.www.himss.org/membership-participation-chapters
- Health Information and Management Systems Society. (n.d.-b). Technology Informatics Guiding Education Reform (TIGER): An initiative for technology and health informatics education.www.himss.org/professionaldevelopment/tiger-initiative
- Health Information and Management Systems Society. (2017). HIMSS 2017 nursing informatics workforce survey. www.himss.org/sites/hde/files/d7/2017-nursing-informatics-workforce-full-report.pdf
- Health Information and Management Systems Society. (2020). 2020 nursing informatics workforce survey. www.himss.org/sites/hde/files/media/file/2020/05/15/himss_nursinginformaticssurvey2020_v4.pdf
- Holden R. J., Binkheder S., Patel J., & Viernes S. (2018). Best practices for health informatician involvement in interprofessional health care teams. Applied Clinical Informatics, 9(1), 141-148. https://doi.org/10.1055/s-0038-1626724
- Hunter K. M., McGonigle D., & Hebda T. (2012, June-23). Operationalizing TIGER NI competencies for online assessment of perceived competency. 11th International Congress on Nursing Informatics, Montreal, Canada.
- Hunter K., McGonigle D., & Hebda T. (2013). TIGER-based measurement of nursing informatics competencies: The development and implementation of an online tool for self-assessment. Journal of Nursing Education and Practice, 3(12), 70-80. https://dx.doi.org/10.5430/jnep.v3n12p70
- Hunter K., McGonigle D., Hebda T., Sipes C., Hill T., & Lamblin J. (2015). TIGER-based assessment of nursing informatics competencies (TANIC). In A.Rocha , S.Correia , S.Costanza , & L.Reis (Eds.), New contributions in information systems and technologies (Vol. 1, pp. 171-177). Springer.
- Institute for Credentialing Excellence. (n.d.). About us. www.credentialingexcellence.org/About
- Kim L. (2020). Cybercrime, ransomware, and the role of the informatics nurse. Nursing, 50(3), 63-65. http://dx.doi.org/10.1097/01.NURSE.0000654064.67531.c5
- Lavin M., Harper E., & Barr N. (2015). Health information technology, patient safety, and professional nursing care documentation in acute care settings. Online Journal of Issues in Nursing, 20(2), 6. doi:10.3912/OJIN.Vol20No02PPT04
- Mack J. (n.d.). Do you need to be certified in health informatics? University of San Diego. https://onlinedegrees.sandiego.edu/do-you-need-health-informatics-certification
- McGonigle D., Hunter K., Hebda T., & Hill T. (2013). Assessment of level 3 and level 4 nursing informatics (NI) competencies tool development. https://sigma.nursingrepository.org/bitstream/handle/10755/623941/ToolAssessment.pdf?sequence=1&isAllowed=y
- McGonigle D., Hunter K., Hebda T., Sipes C., Hill T., & Lamblin J. (2015). Nursing informatics competencies assessment level 3 and level 4 (NICA L3/L4). In A.Rocha , S.Correia , S.Costanza , & L.Reis (Eds.), New contributions in information systems and technologies (Vol. 1, pp. 209-214). Springer.
- McNeil B. J., Elfrink V., Beyea S. C., Pierce S., & Bickford C. J. (2006). Computer literacy study: Report of qualitative findings. Journal of Professional Nursing, 22(1), 52-59. https://doi.org/10.1016/j.profnurs.2005.12.006
- Saba V. K., & McCormick K. A. (Eds.). (2006). Essentials of nursing informatics (4th ed.). McGraw-Hill.
- Staggers N., Gassert C., & Curran C. (2001). Informatics competencies for nurses at four levels of practice. Journal of Nursing Education, 40(7), 303-316. https://doi.org/10.3928/0148-4834-20011001-05
- Staggers N., Gassert C., & Curran C. (2002). A Delphi study to determine informatics competencies for nurses at four levels of practice. Nursing Research, 51(6), 383-390. https://doi.org/10.1097/00006199-200211000-00006
- Thede L. Q. (2003). Informatics and nursing: Opportunities and challenges (2nd ed.). Lippincott Williams & Wilkins.
- Topkaya S., & Kaya N. (2015). Nurses' computer literacy and attitudes towards the use of computers in health care. Journal of Nursing Interventions, 21(S2), 141-149. http://dx.doi.org/10.1111/ijn.12350