Acute liver failure (ALF) is defined as the rapid progression of liver dysfunction resulting in coagulopathy and altered mentation in patients without previously known liver disease. Practically, it is described as the constellation of acute severe hepatic injury (<26 wk); synthetic liver dysfunction, specifically coagulopathy (international normalized ratio [INR] >1.5); and any degree of mental alteration (encephalopathy) in a patient without preexisting cirrhosis and in the absence of acute alcoholic hepatitis. ALF can also be diagnosed in patients with preexisting liver disease, such as Wilson disease, vertically acquired hepatitis B, and autoimmune hepatitis (despite the possibility of cirrhosis in these patients), provided that diagnosis of these conditions was made within the preceding 26 wk.1Box 1 summarizes classifications of ALF. ALF must be distinguished from acute-on-chronic liver failure and acutely decompensated cirrhosis, two syndromes that pertain to acute deterioration in patients with preexisting chronic liver disease.2 Acutely decompensated cirrhosis refers to the development of ascites, encephalopathy, gastrointestinal hemorrhage, or any combination of these disorders in patients with cirrhosis.1 Acute-on-chronic liver failure is a syndrome where acute and severe hepatic derangements occur secondary to various insults in patients with chronic liver disease, including both cirrhotic and non-cirrhotic. It occurs in the context of intense systemic inflammation (e.g., infections or alcoholic hepatitis) and can be associated with single or multiorgan failure.2,3
BOX 1 Classifications of Acute Liver Failure
HE, Hepatic encephalopathy.From Vincent JL et al: Textbook of critical care, ed 7, Philadelphia, 2017, Elsevier.
Acute and subacute necrosis of liver
| ||||||||||||||||||||
Affects approximately 2000 people/yr in U.S. and 1 to 8 people per million population in the U.K.1
- Clinical Presentation Initial symptoms of ALF are mostly nonspecific and depend on the etiology of liver injury. They include fatigue, lethargy, anorexia, and nausea/vomiting. Pruritus, jaundice, and right upper quadrant abdominal pain and distention may be present. Symptoms may also be more serious and consist of severe hypotension, sepsis, and hepatic encephalopathy.
- Physical Examination Findings include, by definition, abnormal neurologic findings of encephalopathy (see Table 1). Other findings may include jaundice, asterixis, hepatomegaly, decreased hepatic mass on percussion, and ascites. Multisystem organ failure can ensue. In rare cases, as the hepatic encephalopathy progresses, cerebral edema and increased intracranial pressure can occur, with abnormal pupillary exam findings, hypertension, bradycardia, respiratory depression (Cushing triad), and loss of brain stem reflexes. Seizures secondary to increased intracranial pressure and hypoxia can occur. Vesicular skin lesions are suggestive of HSV.
- Family history of unexplained liver disease/cirrhosis should prompt slit lamp ocular examination for the identification of Kayser-Fleischer rings (copper rings around the iris seen in Wilson disease).
TABLE 1 Features Distinguishing Acute Liver Failure from Chronic Hepatic Encephalopathy or Portal Systemic Encephalopathy
| Feature | Acute Liver Failure | Portal Systemic Encephalopathy |
|---|---|---|
| History | ||
| Onset | Usually acute | Varies; may be insidious or subacute |
| Mental state | Mania may evolve to deep coma | Blunted consciousness |
| Precipitating factor | Viral infection or hepatotoxin | Gastrointestinal hemorrhage, exogenous protein, drugs, uremia, infection |
| History of liver disease | No | Usually yes |
| Symptoms | ||
| Nausea, vomiting | Common | Unusual |
| Abdominal pain | Common | Unusual |
| Signs | ||
| Liver | Small, soft, tender | Usually large, firm, no pain |
| Nutritional state | Normal | Cachectic |
| Collateral circulation | Absent | May be present |
| Ascites | Absent | May be present |
| Laboratory Test | ||
| Transaminases | Very high | Normal or slightly high |
| Coagulopathy | Present | Often present |
From Jankovic J et al: Bradley and Daroff’s neurology in clinical practice, ed 8, Philadelphia, 2022, Elsevier.
Other, more rare causes include alcoholic hepatitis, autoimmune hepatitis, Wilson disease, ischemic hepatopathy, Budd-Chiari syndrome, acute fatty liver of pregnancy, venoocclusive disease, toxin ingestion (e.g., mushroom poisoning [Amanita phalloides]), sepsis, infiltrative malignancy (breast cancer, lymphoma, myeloma, melanoma, small cell lung cancer), and other viruses (adenovirus, hepatitis E, herpes simplex virus [HSV]). Box 2 summarizes possible etiologies of liver failure.
- Coagulopathy is characteristic of patients with ALF, given decreased synthesis of clotting factors II, V, VII, IX, and X by the liver. Patients with ALF typically have a prolonged prothrombin time (INR >1.5), elevated transaminases, and elevated bilirubin, and may have a low platelet count (<150,000).
- Other possible laboratory findings can include an elevated blood urea nitrogen (BUN)/creatinine (studies show 30% to 50% also have acute kidney injury) and hypoglycemia (impairment of gluconeogenesis). Electrolyte disturbances, hyponatremia, hypophosphatemia, hypomagnesemia, hypokalemia, metabolic acidosis or respiratory alkalosis, elevated lactate dehydrogenase, and elevated ammonia.
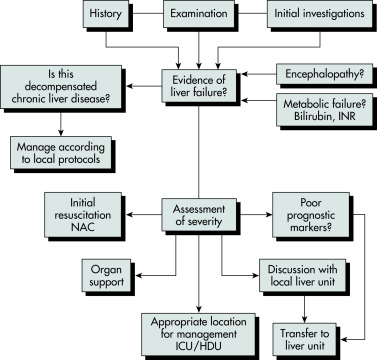
Broadly, the treatment of ALF should include:
- Identification of the etiology of liver injury, if possible, and specific treatment
- Symptomatic and supportive management and transfer to an intensive care unit (ICU) if necessary
- Early involvement of a liver specialist and transfer to a transplant center when required
BOX 5 Hepatic Replacement Therapeutic Options Available to Patients with Fulminant Hepatic Failure
From Vincent JL et al: Textbook of critical care, ed 6, Philadelphia, 2011, Saunders.
BOX 4 Management of Fulminant Hepatic Failure
No sedation except for procedures Enteric precautions until infection ruled out
Maintain circulating volume with colloid/FFP Coagulation support only if required
|
BP, Blood pressure; CVP, central venous pressure; PT, prothrombin time; PTT, partial thromboplastin time; FFP, fresh frozen plasma; PN, parenteral nutrition.From Fuhrman BP, Zimmerman JJ: Fuhrman and Zimmerman’s pediatric critical care, ed 4, Philadelphia, 2011, Mosby.