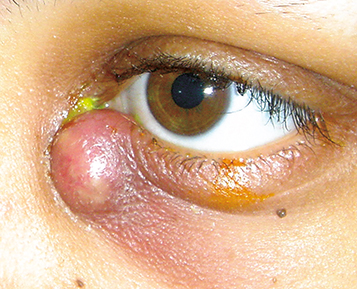
(see Figure 6.11.1.)
Erythematous, tender, tense swelling over the nasal aspect of the lower eyelid and extending around the periorbital area. Mucoid or purulent discharge may be expressed from the punctum when pressure is applied over the lacrimal sac, although this is not necessary nor sufficient for diagnosis.
Swelling in dacryocystitis is below the medial canthal tendon. Suspect lacrimal sac tumor (rare) if the mass is above the medial canthal tendon. |
Fistula formation may occur between the skin and the lacrimal sac. A lacrimal sac cyst or mucocele can occur in chronic cases. Progression to a lacrimal sac abscess, and rarely, orbital or facial cellulitis may occur.