Decreased vision, pain, tearing, foreign body sensation, photophobia, and redness. History of cataract surgery in the involved eye.
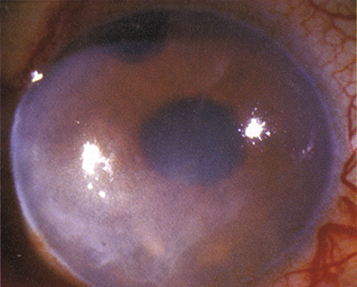
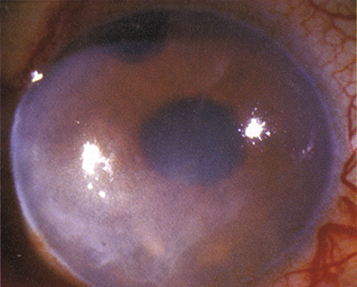
(See Figure 4.28.1.)
Figure 4.28.1: Pseudophakic bullous keratopathy.
Critical
Corneal edema in an eye in which the native lens has been removed.
Other
Corneal bullae, Descemet folds, subepithelial haze or scarring, corneal neovascularization, with or without preexisting guttae. Cystoid macular edema (CME) may be present.
Multifactorial: Corneal endothelial damage, intraocular inflammation, vitreous or subluxed intraocular lens or tube shunt touching (or intermittently touching) the cornea, preexisting endothelial dysfunction, and glaucoma.
If ruptured bullae, every 1 to 3 days until improvement demonstrated, and then every 5 to 7 days until the epithelial defect heals. Otherwise, every 1 to 6 months, depending on symptoms.