Mild photophobia, mild pain, localized red eye, chronic eyelid crusting, foreign body sensation, or dryness. History of recurrent acute episodes, chalazia, or styes.
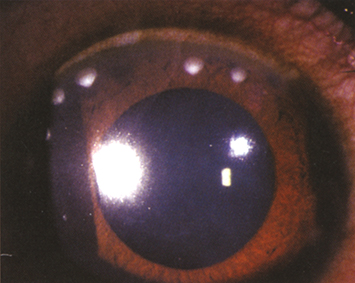
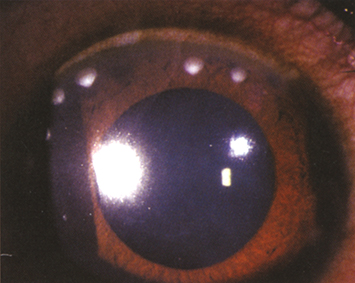
(See Figure 4.19.1.)
Figure 4.19.1: Staphylococcal hypersensitivity.
Critical
Singular or multiple, unilateral or bilateral, peripheral corneal stromal infiltrates often with a clear space between the infiltrates and the limbus. Variable staining with fluorescein. Minimal anterior chamber inflammation. Sectoral conjunctival injection typically occurs.
Other
Blepharitis, inferior SPK, phlyctenule (a wedge-shaped, raised, vascularized sterile infiltrate near the limbus, usually in children). Peripheral scarring and corneal neovascularization. Findings often present in the contralateral eye or elsewhere in the affected eye.
Infiltrates are believed to be a cell-mediated, or delayed, type IV hypersensitivity reaction to bacterial antigens in the setting of staphylococcal blepharitis.
|
 NOTE NOTEPatients with ocular rosacea (e.g., meibomian gland inflammation and telangiectasias of the eyelids) are especially susceptible to this condition. |
Mild
Warm compresses, eyelid hygiene, an antibiotic drop q.i.d. (e.g., fluoroquinolone or trimethoprim/polymyxin B), and an antibiotic ophthalmic ointment q.h.s. (e.g., bacitracin, erythromycin, bacitracin/polymyxin B). See 5.8, Blepharitis/Meibomitis.
Moderate to Severe
Treat as described for mild but add a low-dose topical steroid (e.g., loteprednol 0.5%, fluorometholone 0.1%, or prednisolone acetate 0.125% q.i.d.) with an antibiotic (e.g., fluoroquinolone or trimethoprim/polymyxin B q.i.d.). A combination antibiotic/steroid can also be used q.i.d. (e.g., loteprednol 0.5%/tobramycin 0.3%, dexamethasone 0.1%/tobramycin 0.3%, or dexamethasone 0.05%/tobramycin 0.3%). Steroid use without antibiotic coverage is not recommended. Maintain until the symptoms improve and then slowly taper.
If episodes recur despite eyelid hygiene, add systemic doxycycline (50 to 100 mg daily for 1 to 3 months) until the ocular disease is controlled. This medication has an anti-inflammatory effect on the sebaceous glands in addition to its antimicrobial action. Topical azithromycin q.h.s., erythromycin q.h.s., or cyclosporine b.i.d. may be helpful in controlling eyelid inflammation.
Low-dose antibiotics (e.g., bacitracin or erythromycin ointment q.h.s.) may have to be maintained indefinitely.
|
 NOTE NOTETetracyclines such as doxycycline are contraindicated in children <8 years old, pregnant women, and breastfeeding mothers. Erythromycin 200 mg p.o. one to two times per day can be used in children to decrease recurrent disease. |
In 2 to 7 days, depending on the clinical picture. IOP is monitored while patients are taking topical steroids.