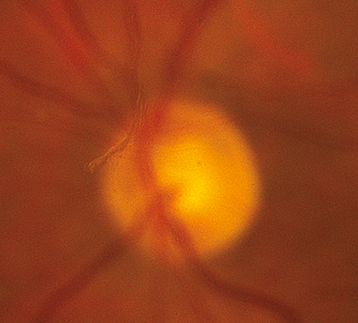
One or more discrete near-translucent or light gray vitreous opacities, one often in the shape of a ring (“Weiss ring”) or broken ring, suspended over the optic disc (See Figure 11.1.1).
Retinal break/tear (RT), retinal detachment (RD), pigmented cells in the anterior vitreous (“tobacco dust” or Shafer sign), or vitreous hemorrhage (VH) may occur with or without a posterior vitreous detachment (PVD), with similar symptoms. Peripheral retinal and disc margin hemorrhages.
Approximately 10% of all patients with acute symptomatic PVD have a retinal break. The presence of pigmented cells in the anterior vitreous or VH in association with an acute PVD indicates a high probability (>70%) of a coexisting retinal break. See 11.2, Retinal Break (Tear). |