Definition
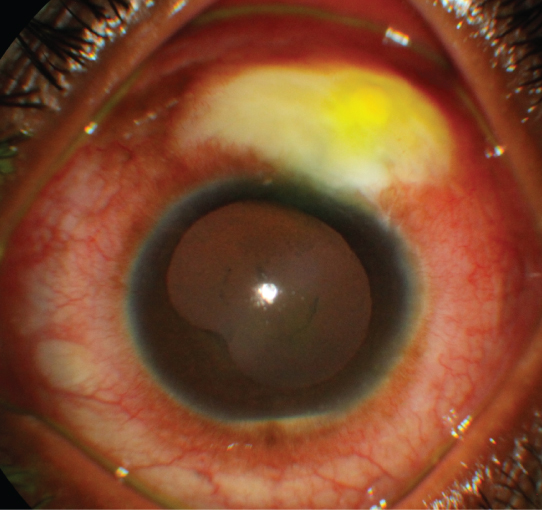
Infection of a filtering bleb. May occur any time after glaucoma filtering procedures (days to years). Greater incidence with use of antimetabolites during initial surgery, multiple surgeries, and postoperative complications including flat anterior chamber and wound leak.
Grade 1 (mild): Bleb infection, hyperemia or purulence, but no anterior chamber or vitreous involvement.
Grade 2 (moderate): Bleb infection with anterior chamber inflammation but no vitreous involvement.
Grade 3 (severe): Bleb infection with anterior chamber and vitreous involvement. See 12.14, Acute Postoperative Endophthalmitis and12.15, Subacute and Chronic Postoperative Endophthalmitis.
Red eye and discharge early. Later, aching pain, photophobia, decreased vision, and mucous discharge.
Daily until infection is resolving. Hospital admission may be indicated.
REFERENCE
RazeghinejadMR, HavensS, KatzLJ. Trabeculectomy bleb-associated infection. Surv Ophthalmol. 2017;62(5):591–610.