Sharp pain, photophobia, foreign body sensation, tearing, discomfort with blinking or eye movement, redness, blurred vision, and history of scratching or hitting the eye.
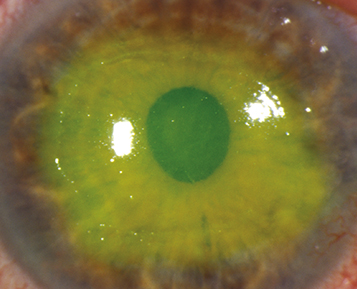
(See Figure 3.3.1.)
Epithelial defect that stains with fluorescein; absence of underlying corneal opacification (presence of which indicates infection or inflammation).
Conjunctival injection, swollen eyelid, and mild AC reaction.
Recurrent erosion (see 4.2, Recurrent Corneal Erosion).
Herpes simplex keratitis (see 4.16, Herpes Simplex Virus).
Confluent SPK (see 4.1, Superficial Punctate Keratopathy).
Ultraviolet keratopathy (see 4.7, Ultraviolet Keratopathy).
Exposure keratopathy (see 4.5, Exposure Keratopathy).
Neurotrophic keratopathy (see 4.6, Neurotrophic Keratopathy).
Chemical burn (see 3.1, Chemical Burn).
Thermal injury (see 3.2, Thermal Injuries).
Slit-lamp examination: Use fluorescein dye, measure the size (e.g., height and width) of the abrasion, and diagram its location. Evaluate for foreign body, infiltrate (underlying corneal opacification), AC reaction, hyphema, corneal laceration, and penetrating trauma.
Evert the eyelids to ensure that no foreign body is present, especially in the presence of vertical or linear abrasions.
Noncontact lens wearer: Antibiotic ointment (e.g., erythromycin, bacitracin, or bacitracin/polymyxin B q2–4h while awake) or antibiotic drops (e.g., polymyxin B/trimethoprim or a fluoroquinolone q.i.d.). Abrasions secondary to fingernails or vegetable matter should be covered with a fluoroquinolone drop (e.g., ofloxacin, moxifloxacin, besifloxacin) or ointment (e.g., ciprofloxacin) at least q.i.d.
Contact lens wearer: Must have antipseudomonal coverage (e.g., fluoroquinolone). Should use antibiotic ointment or antibiotic drops at least q.i.d.
Cycloplegic agent (e.g., cyclopentolate 1% to 2% b.i.d. or t.i.d.) for traumatic iritis, which may develop 24 to 72 hours after trauma. Avoid steroid use for iritis with epithelial defects because it may impede epithelial healing and increase infection risk. Avoid use of long-acting cycloplegics for small abrasions to allow for faster visual recovery.
Patching is rarely necessary and can cause a serious abrasion if not applied properly. Patching should be avoided in all contact lens–related corneal abrasions due to higher risk of infection.
Consider a short course of topical nonsteroidal anti-inflammatory drug (NSAID) drops (e.g., ketorolac 0.4% to 0.5% q.i.d. for 3 days) for pain control. Avoid in patients with other ocular surface diseases. Oral acetaminophen, NSAIDs, or narcotics (in severe cases) can also be used for pain control.
Debride loose or hanging epithelium because it may inhibit healing. A cotton-tipped applicator soaked in topical anesthetic (e.g., proparacaine) or sterile jeweler’s forceps (used with caution) may be utilized.
Bandage contact lenses may be used to improve comfort and protect the epithelium during healing. Contact lenses are rarely used in the emergency room setting out of concern for patient compliance and follow-up. If a bandage contact lens is placed, patients should use prophylactic topical antibiotics (e.g., polymyxin B/trimethoprim or a fluoroquinolone q.i.d.) and should be monitored closely for epithelial healing and contact lens replacement. Do not use for abrasions associated with contact lens wear or if any concern for infection exists.
Never prescribe topical anesthetics (e.g., proparacaine, tetracaine) for analgesia, as this may delay epithelial healing and increase infection and ulceration risk. |
If patched or given bandage contact lens, the patient should return in 24 hours (or sooner if symptoms worsen) for reevaluation.
Central or large corneal abrasion: Return the next day to determine if the epithelial defect is improving. If the abrasion is healing, may see 2 to 3 days later. Instruct patient to return sooner if symptoms worsen. Revisit every 3 to 5 days until healed.
Peripheral or small abrasion: Return 2 to 5 days later. Instruct patient to return sooner if symptoms worsen. Revisit every 3 to 5 days until healed.
Close follow-up until the epithelial defect resolves, and then treat with topical antibiotic (e.g., fluoroquinolone drops) for an additional 1 or 2 days. The patient may resume contact lens wear after the eye feels normal for a week after cessation of a proper medication course. A new contact lens should be used at that time.