A.6. What are the basic principles of echocardiography? What are M-mode, B-mode, and Doppler color modalities? How are pressure gradients measured by echocardiography? How do TTE and transesophageal echocardiography (TEE) differ?
Answer:
Echocardiography is the use of ultrasound waves to image structures and blood flow within the heart and great vessels. To image tissue, sound waves are emitted from a transducer at known speeds and constant intervals. The sound packets bounce off structures in their path, and the reflected sound waves are received by the transducer during its "listening" mode. The time it takes for the reflected waves to return to the crystal is measured, and because the velocity of sound in tissues is relatively constant (1,540 m/s), solving for distance can be easily accomplished:
Distance = ½ (Velocity × Time)
(½ because the distance is traversed twice, once to the object and again on returning).
In this manner, the spatial orientation of cardiac structures can be determined. The strength of the returning signal can be quantified as an amplitude, thus "A" or amplitude mode (Figure 7.12B). The echocardiographic system codes this amplitude on a black and white scale, thereby converting the amplitude to brightness or B-mode scanning (Figure 7.12C). Figure 7.12D shows this "ice-pick" view through the LV of the heart. Each change in tissue density results in some sound waves being reflected and hence an interface. In this example, bold lines are seen at the epicardial, the endocardial-chamber, the chamber-endocardial, and the epicardial borders. If these amplitude bars are displayed in real time, then a motion or M-mode display results (Figure 7.12E). These images were difficult to obtain and interpret reliably because the views represent a linear slice without surrounding structural images for referencing. If the probe is moved in a sweeping mode, back and forth repetitively, then multiple M-mode images can be obtained in a given instant and a two-dimensional (2D) image formed. This rapid back-and-forth sweep of the ultrasound beam is performed electronically in a phased array transducer. The images derived in this manner appear as a cineradiographic display of myocardial movement. Echocardiography can provide information about the size, shape, location, and movement of myocardial structures.
Figure 7.12.: The Process of Producing the B-Mode and M-Mode Images.
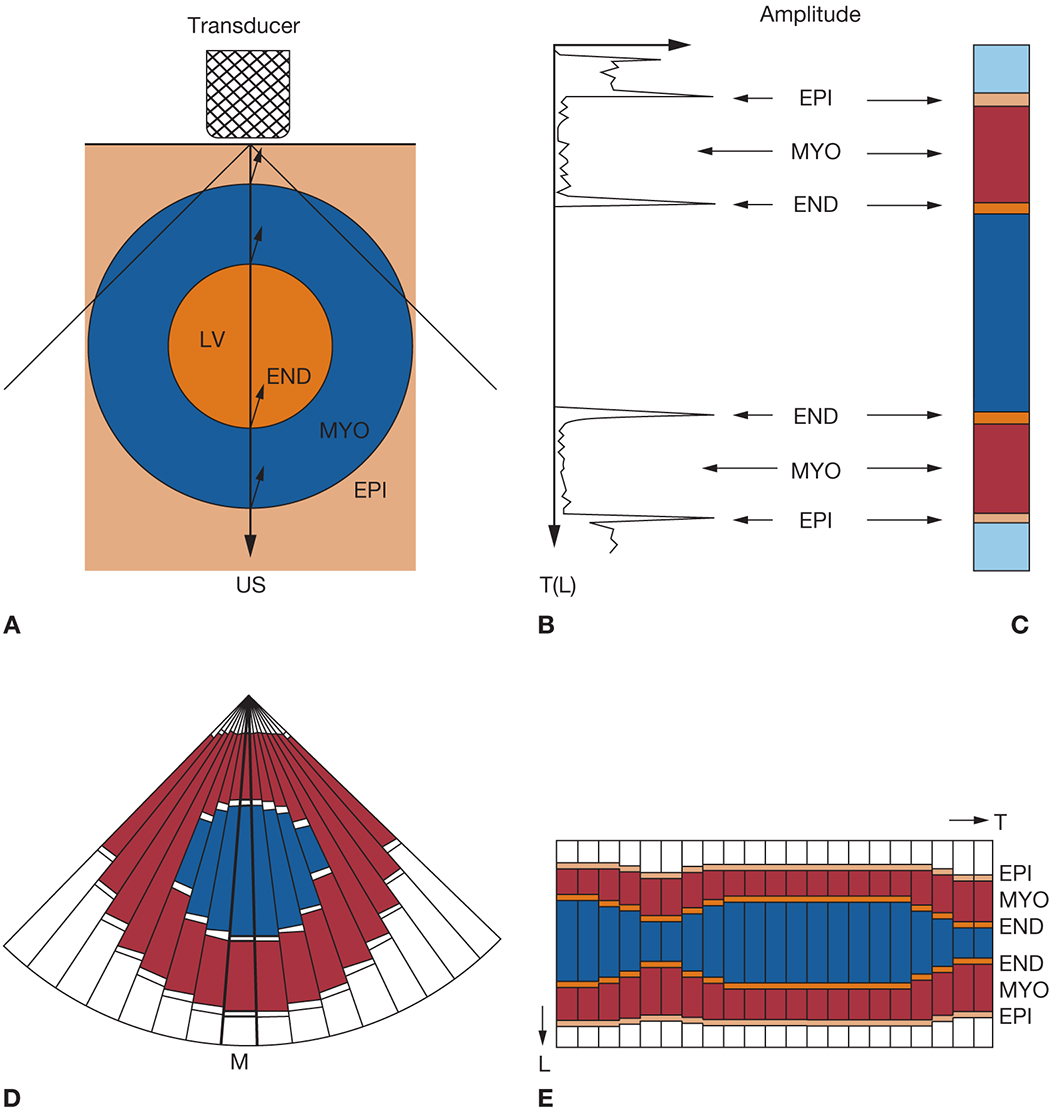
The process of producing the B-mode and M-mode images. A. A pulse of ultrasound is emitted into the object, and the backscattered echo is received by the same transducer. B. The received acoustic signal is converted to the electric signal (A-mode). C. The amplitude is modulated into brightness (B-mode). D. As subsequent pulses of ultrasound are emitted with the sequentially changing angles and the obtained one-dimensional (1D) B-mode images are compounded according to the direction of each ultrasound emission, the first frame of the sector-shaped image is formed. E. When the ultrasound is repeatedly transmitted in one direction, a series of 1D B-mode images is obtained. As these are arranged against time, an M-mode image is obtained. END, endocardium; EPI, epicardium; L, length; LV, left ventricle; M, motion; MYO, myocardium; T, time; US, ultrasound. (Reprinted with permission from Oka Y, Goldiner PL, eds. Transesophageal Echocardiography. JB Lippincott; 1992:12.)
Contact of the sound wave packet with the reflecting object (tissue, blood cells, air) also alters the wavelength of the sound packet according to the Doppler principle. When the reflecting object is moving toward the source of the ultrasound, the reflected ultrasound wavelengths are compressed (shorter). The opposite occurs when the object is moving away from the sound source. These shifts in frequency (ΔF) are proportional to the velocity of the contacted structure, and thereby, the velocity and direction of the encountered object (usually of blood flow) can be calculated. With Doppler ultrasound, only the component of blood flow parallel to the Doppler beam will be analyzed because the Doppler equation, velocity = c (ΔF) / 2 FT(cos θ), contains the cosine of the angle of incidence between the ultrasound beam and the moving object (FT is the transmitted frequency). Because the cosine of 90° is zero, blood flow that is perpendicular to the ultrasound beam will not cause a Doppler shift and therefore cannot be measured. It is important to choose an ultrasound "window" in which the expected blood flow direction is most parallel to the ultrasound. This velocity information can be displayed on a color map (Doppler color flow) or on a time/velocity scale (spectral Doppler display). Doppler-derived blood flow velocity information can identify laminar and turbulent flow patterns, regurgitant or stenotic lesions, and congenital anomalies and can permit quantification of pressure gradients.
Pressure gradients (ΔP) can be estimated from the measured blood flow velocity using the modified Bernoulli equation (ΔP = 4 × velocity2). Simply put, the greater the velocity of blood flow, the higher is the ΔP. TTE uses imaging points or "acoustic windows" obtained with the transducer handheld on the chest wall. TTE is simple and noninvasive. Most standard echocardiograms are obtained from this position. During cardiac surgery, the chest wall is in the sterile field and therefore unavailable. The esophagus lies immediately adjacent to the heart outside of the operative field and affords an excellent imaging vantage point. The close proximity of the probe to the heart affords excellent resolution. The probe is not in the operative field, so surgery is unhindered and sterility is not at risk.
Intraoperative TEE is beneficial for quantification of cardiac contractility, for determination of the severity of regurgitant and stenotic valvular disease, for detection of intracardiac shunts and the occurrence of dissections, and as a guide for catheter and cannula placement. Accordingly, intraoperative TEE is now standard of care for open heart (eg, valve) operations, as well as a wide array of percutaneous cardiac interventions. Although invasive, the risk for esophageal injury in the anesthetized state is low. Nonetheless, prior to TEE, all patients should be screened for history of esophageal disease (eg, prior esophageal surgery, strictures or varices) or symptoms suggestive of esophageal pathology that can increase risk of injury from the probe.
References
- American Society of Anesthesiologists and Society of Cardiovascular Anesthesiologists Task Force on Transesophageal Echocardiography. Practice guidelines for perioperative transesophageal echocardiography. An updated report by the American Society of Anesthesiologists and the Society of Cardiovascular Anesthesiologists Task Force on Transesophageal Echocardiography. Anesthesiology. 2010;112:1084-1096.
- Otto CM. Principles of echocardiographic image acquisition and doppler analysis. In: Otto CM, ed. Textbook of Clinical Echocardiography. 6th ed. Elsevier; 2018:1-32.


