Causes are outlined in Table 1-4; in most cases, hyperkalemia is due to decreased renal K+ excretion. However, increases in dietary K+ intake can have a major effect in susceptible pts, e.g., diabetics with hyporeninemic hypoaldosteronism and chronic kidney disease (CKD). Drugs that impact on the RAA axis are also a major cause of hyperkalemia.
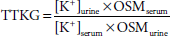
The first priority in the management of hyperkalemia is to assess the need for emergency treatment (ECG changes and/or K+≥6.0 mM). This should be followed by a comprehensive workup to determine the cause (Fig. 1-3). History and physical examination should focus on medications (e.g., ACE inhibitors, NSAIDs, trimethoprim/sulfamethoxazole), diet and dietary supplements (e.g., salt substitute), risk factors for acute kidney failure, reduction in urine output, blood pressure, and volume status. Initial laboratory tests should include electrolytes, BUN, creatinine, serum osmolality, Mg2+, and Ca2+, a complete blood count, and urinary pH, osmolality, creatinine, and electrolytes. A urine [Na+] <20 meq/L suggests that distal Na+ delivery is a limiting factor in K+ excretion; volume repletion with 0.9% saline or treatment with furosemide may then be effective in reducing serum [K+] by increasing distal Na+ delivery. Serum and urine osmolality are required for calculation of the TTKG. The expected values of the TTKG are largely based on historic data: <3 in the presence of hypokalemia and >7-8 in the presence of hyperkalemia.
Treatment: Hyperkalemia The most important consequence of hyperkalemia is altered cardiac conduction, with the risk of bradycardic cardiac arrest. Figure 1-4 shows serial ECG patterns of hyperkalemia; ECG manifestations of hyperkalemia should be considered a true medical emergency and treated urgently. However, ECG changes of hyperkalemia are notoriously insensitive, particularly in pts with CKD; given these limitations, pts with significant hyperkalemia (K+≥6-6.5 mmol/L) in the absence of ECG changes should also be aggressively managed. Urgent management of hyperkalemia constitutes a 12-lead ECG, admission to the hospital, continuous cardiac monitoring, and immediate treatment. Treatment of hyperkalemia is divided into three categories: (1) antagonism of the cardiac effects of hyperkalemia, (2) rapid reduction in [K+] by redistribution into cells, and (3) removal of K+ from the body. Treatment of hyperkalemia is summarized in Table 1-5. |