Early recognition and immediate treatment of acute ST-segment elevation myocardial infarction (STEMI) are essential; diagnosis is based on characteristic history, ECG, and serum cardiac biomarkers.
Symptoms
Chest pain similar to angina (Chap. 33 Chest Pain) but more intense and persistent; not fully relieved by rest or nitroglycerin, often accompanied by nausea, sweating, apprehension. However, 20-25% of MIs are clinically silent.
Physical Examination
Pallor, diaphoresis, tachycardia, S4, dyskinetic cardiac impulse may be present. If heart failure exists, pulmonary crackles and S3 may be present. Jugular venous distention is common in right ventricular infarction.
ECG
ST elevation in at least two contiguous leads (≥2 mm in men, or ≥ 1.5 mm in women, in leads V2-V3, or ≥1 mm in other leads), followed (if acute reperfusion is not achieved) by T-wave inversion then Q-wave development over several hours.
Cardiac Biomarkers
Cardiac-specific troponins T and I are highly specific for myocardial injury and are the preferred biochemical markers for diagnosis of acute MI. Serum levels remain elevated for 7-10 days. Creatine kinase (CK), another biomarker (which is not necessary to measure if cardiac troponin is assessed) rises within 4-8 h, peaks at 24 h, and returns to normal by 48-72 h. CK-MB isoenzyme is more specific for MI than total CK (which may be elevated in skeletal muscle injury). The decision to proceed with reperfusion therapies in acute STEMI should be made urgently from the pt's history and ECG, and not await the results of biomarker assays.
Noninvasive Imaging Techniques
May be useful when diagnosis of MI is not clear. Echocardiography detects infarct-associated regional wall motion abnormalities (but cannot distinguish acute MI from a previous myocardial scar). Echo is also useful in detecting RV infarction, LV aneurysm, and LV thrombus. MRI with delayed gadolinium enhancement accurately indicates regions of infarction, but is technically difficult to perform in acutely ill pts.
| TREATMENT | ||
STEMIINITIAL THERAPYInitial goals are to (1) quickly identify if pt is candidate for reperfusion therapy, (2) relieve pain, and (3) prevent/treat arrhythmias and mechanical complications.
The initial management of NSTEMI (non-Q MI) is different (Chap. 122 Unstable Angina and Non-ST-Elevation Myocardial Infarction). In particular, fibrinolytic therapy should not be administered. ADDITIONAL STANDARD TREATMENT(Whether or not reperfusion therapy is undertaken):
|
Complications
(For arrhythmias, see also Chaps. 124 Bradyarrhythmias and 125 Tachyarrhythmias.)
Isolated ventricular premature beats (VPBs) occur frequently. Precipitating factors should be corrected (hypoxemia, acidosis, hypokalemia, hypomagnesemia, CHF, arrhythmogenic drugs). Routine beta blocker administration (see above) diminishes ventricular ectopy. Other in-hospital antiarrhythmic therapy should be reserved for pts with sustained ventricular arrhythmias.
If hemodynamically unstable, perform immediate electrical countershock (unsynchronized discharge of 200-300 J or 50% less if using biphasic device). If hemodynamically tolerated, use IV amiodarone (bolus of 150 mg over 10 min, then infusion of 1.0 mg/min for 6 h, then 0.5 mg/min).
Ventricular Fibrillation (VF) 
VF requires immediate defibrillation (200-400 J). If unsuccessful, initiate cardiopulmonary resuscitation (CPR) and standard resuscitative measures (Chap. 11 Cardiovascular Collapse and Sudden Death). Ventricular arrhythmias that appear several days or weeks following MI often reflect pump failure and may warrant invasive electrophysiologic study and implantation of a cardioverter defibrillator (ICD).
Accelerated Idioventricular Rhythm 
Wide QRS complex, regular rhythm, rate 60-100 beats/min, is common and usually benign; if it causes hypotension, treat with atropine 0.6 mg IV.
Supraventricular Arrhythmias 
Sinus tachycardia may result from heart failure, hypoxemia, pain, fever, pericarditis, hypovolemia, administered drugs. If no cause is identified, suppressive beta blocker therapy may be beneficial to reduce myocardial oxygen demand. Other supraventricular arrhythmias (paroxysmal supraventricular tachycardia, atrial flutter, and fibrillation) are often secondary to heart failure. If hemodynamically unstable, proceed with electrical cardioversion. In absence of acute heart failure, suppressive alternatives include beta blockers, verapamil, or diltiazem (Chap. 125 Tachyarrhythmias).
(See Chap. 124 Bradyarrhythmias.) In inferior MI, usually represent heightened vagal tone or discrete AV nodal ischemia. If hemodynamically compromised (CHF, hypotension, emergence of ventricular arrhythmias), treat with atropine 0.5 mg IV q5min (up to 2 mg). If no response, use temporary external or transvenous pacemaker. Isoproterenol should be avoided. In anterior MI, AV conduction defects usually reflect extensive tissue necrosis. Consider temporary external or transvenous pacemaker for (1) complete heart block, (2) Mobitz type II block (Chap. 124 Bradyarrhythmias), (3) new bifascicular block (LBBB, RBBB + left anterior hemiblock, RBBB + left posterior hemiblock), (4) any bradyarrhythmia associated with hypotension or CHF.
CHF may result from systolic “pump” dysfunction, increased LV diastolic “stiffness,” and/or acute mechanical complications.
| TREATMENT | ||
Heart FailureInitial therapy includes diuretics (begin with furosemide 10-20 mg IV), inhaled O2, and vasodilators, particularly nitrates (PO, topical, or IV [Chap. 126 Heart Failure and Cor Pulmonale] unless pt is hypotensive [systolic bp <100 mmHg]); digitalis is usually of little benefit in acute MI (See Chap. 126 Heart Failure and Cor Pulmonale). Diuretic, vasodilator, and inotropic therapy (Table 121-1 IV VASODILATORS AND INOTROPIC DRUGS USED IN ACUTE MI) may be guided by invasive hemodynamic monitoring (Swan-Ganz pulmonary artery catheter, arterial line), particularly in pts with accompanying hypotension (Table 121-2 HEMODYNAMIC COMPLICATIONS IN ACUTE MI; Fig. 121-3. Emergency Management of Cardiogenic Shock and Pulmonary Edema). In acute MI, an acceptable pulmonary capillary wedge (PCW) pressure is 15-20 mmHg; in the absence of hypotension, PCW >20 mmHg is treated with diuretic plus vasodilator therapy (IV nitroglycerin [begin at 10 µg/min] or nitroprusside [begin at 0.5 µg/kg per min]) and titrated to optimize bp, PCW, and systemic vascular resistance (SVR). 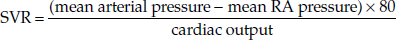 Normal SVR = 900 - 1350 dyne • s/cm5 . If PCW >20 mmHg and pt is hypotensive (Table 121-2 HEMODYNAMIC COMPLICATIONS IN ACUTE MI and Fig. 121-3. Emergency Management of Cardiogenic Shock and Pulmonary Edema), evaluate for VSD or acute mitral regurgitation, consider dobutamine (begin at 1-2 [µg/kg]/min), titrate upward to maximum of 10 (µg/kg)/min; beware of drug-induced tachycardia or ventricular ectopy. After stabilization on parenteral vasodilator therapy, oral therapy follows with an ACE inhibitor or an ARB (Chap. 126 Heart Failure and Cor Pulmonale). Consider addition of long-term aldosterone antagonist (spironolactone 25-50 mg daily or eplerenone 25-50 mg daily) to ACE inhibitor if LVEF ≤40% or symptomatic heart failure or diabetes are present-do not use if renal insufficiency or hyperkalemia are present. |
Cardiogenic Shock
(See Chap. 12. Shock) Severe LV failure with hypotension (bp <90 mmHg), elevated PCW (>20 mmHg), cardiac index <2.2 L/min/m2 , accompanied by oliguria, peripheral vasoconstriction, dulled sensorium, and metabolic acidosis.
| TREATMENT | ||
Cardiogenic ShockSwan-Ganz catheter and intraarterial bp monitoring are not always essential but may be helpful; aim for mean PCW of 18-20 mmHg with adjustment of volume (diuretics or infusion) as needed (Fig. 121-3. Emergency Management of Cardiogenic Shock and Pulmonary Edema). Vasopressors (e.g., norepinephrine or dopamine [Table 121-1 IV VASODILATORS AND INOTROPIC DRUGS USED IN ACUTE MI]) and/or intraaortic balloon counterpulsation may be necessary to maintain systolic bp >90 mmHg and reduce PCW. Administer high concentration of O2 by mask; if pulmonary edema coexists, consider bilateral positive airway pressure (BiPAP) or intubation and mechanical ventilation. Acute mechanical complications (see below) should be sought and promptly treated. If cardiogenic shock develops within 36 h of acute STEMI, reperfusion by PCI or coronary artery bypass grafting (CABG) may markedly improve LV function. |
Hypotension
May also result from right ventricular MI, which should be suspected in inferior or posterior MI, if jugular venous distention and elevation of right-heart pressures predominate (rales are typically absent and PCW may be normal); right-sided ECG leads typically show ST elevation, and echocardiography may confirm diagnosis. Treatment consists of volume infusion. Noncardiac causes of hypotension should be considered: hypovolemia, acute arrhythmia, or sepsis.
Acute Mechanical Complications
Ventricular septal rupture and acute mitral regurgitation due to papillary muscle ischemia/infarct develop during the first week following MI and are characterized by sudden onset of CHF and new systolic murmur. Echocardiography and Doppler interrogation can confirm presence of these complications. PCW tracings may show large v waves in either condition, but an oxygen “step-up” as the catheter is advanced from right atrium to right ventricle suggests septal rupture.
Acute medical therapy of these conditions includes vasodilator therapy (IV nitroprusside: begin at 10 µg/min and titrate to maintain systolic bp ∼100 mmHg); intraaortic balloon pump may be required to maintain cardiac output. Mechanical correction is the definitive therapy. Acute ventricular free-wall rupture presents with sudden loss of bp, pulse, and consciousness, while ECG shows an intact rhythm (pulseless electrical activity); emergent surgical repair is crucial, and mortality is high.
Pericarditis
Characterized by pleuritic, positional pain, and pericardial rub (Chap. 118 Pericardial Disease); atrial arrhythmias are common; must be distinguished from recurrent angina. Often responds to aspirin, 650 mg PO qid. Anticoagulants should be avoided when pericarditis is suspected to avoid development of pericardial bleeding/tamponade.
Ventricular Aneurysm
Localized “bulge” of LV chamber due to infarcted myocardium. True aneurysms consist of scar tissue and do not rupture. However, complications include CHF, ventricular arrhythmias, and thrombus formation. Typically an aneurysm is confirmed by echocardiography or by left ventriculography. The presence of thrombus within the aneurysm, or a large aneurysmal segment due to anterior MI, warrants consideration of oral anticoagulation with warfarin for 3-6 months.
Pseudoaneurysm is a form of cardiac rupture contained by a local area of pericardium and organized thrombus; direct communication with the LV cavity is present; surgical repair usually necessary to prevent rupture.
Recurrent Angina
Usually associated with transient ST-T wave changes; signals high incidence of reinfarction; when it occurs in early post-MI period, coronary arteriography and revascularization should follow.
Secondary Prevention
For pts who have not already undergone coronary angiography and PCI, submaximal exercise testing should be performed prior to or soon after discharge. A positive test in certain subgroups (angina at a low workload, a large region of provocable ischemia, or provocable ischemia with a reduced LVEF) suggests need for cardiac catheterization to evaluate myocardium at risk of recurrent infarction. Beta blockers (e.g., metoprolol, 25-200 mg daily) should be prescribed routinely for at least 2 years following acute MI, unless contraindications present (asthma, active heart failure, bradycardia). Continue oral antiplatelet agents (e.g., aspirin 81-325 mg daily and a P2Y12 platelet receptor antagonist) to reduce incidence of reinfarction. If LVEF ≤40%, an ACE inhibitor or ARB (if ACE inhibitor is not tolerated) should be used indefinitely. Consider addition of aldosterone antagonist (see “Heart Failure ST-Segment Elevation Myocardial Infarction,” above).
Modification of cardiac risk factors must be encouraged: discontinue smoking; control hypertension, diabetes, and serum lipids (typically atorvastatin 80 mg daily in immediate post-MI period-see Chap. 181 Hypercholesterolemia and Hypertriglyceridemia); and pursue graduated exercise.