Tenderness, redness, warmth, and swelling of the eyelid and periorbital area. Often there is a history of local skin abrasions, penetrating injury/trauma, hordeolum, or insect bites. Can be associated with sinusitis, although this is more common with postseptal infections. May complain of fever or chills.
(See Figures 6.10.1 and 6.10.2.)
Critical
Eyelid erythema, tense edema, warmth, and tenderness. No proptosis, no optic neuropathy, no extraocular motility restriction, usually little to no conjunctival injection, and no pain with eye movement (unlike orbital cellulitis). The patient may not be able to open the eye because of eyelid edema. Visual changes such as blurred vision or monocular diplopia attributed to swollen eyelids.
Other
Tightness of eyelid skin or fluctuant eyelid edema. The eye itself may be slightly injected but is relatively uninvolved.
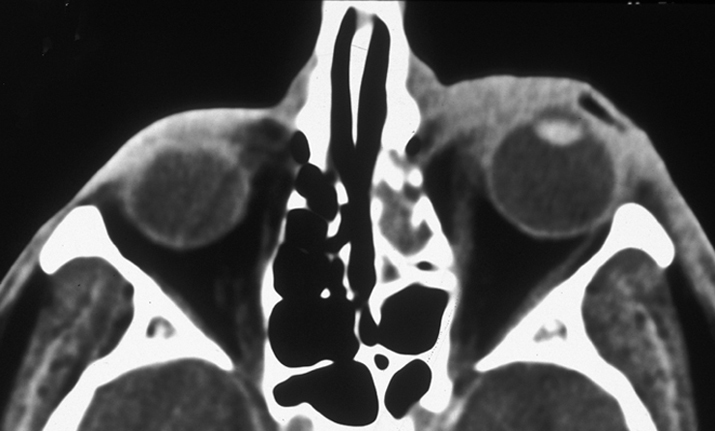
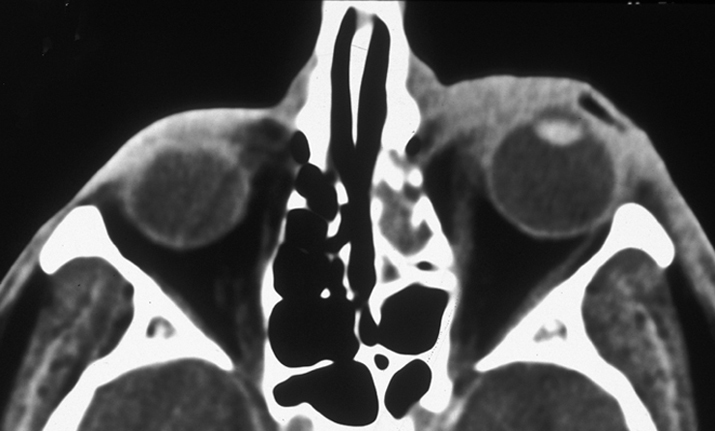
6-10.2 CT of preseptal cellulitis.
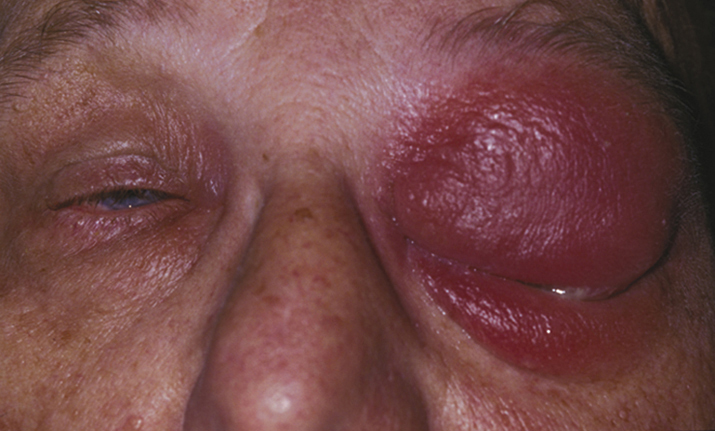
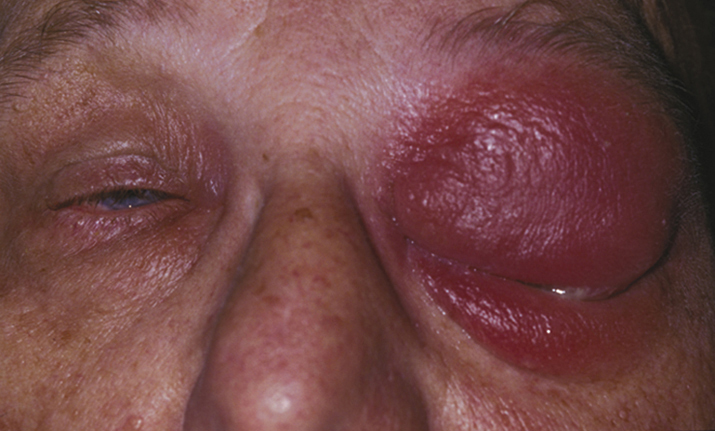
6-10.1 Preseptal cellulitis.
- Adjacent infection (e.g., hordeolum or dacryocystitis).
- Trauma (e.g., puncture wound, laceration, insect bite).
Organisms
S. aureus and Streptococcus are most common, but H. influenzae should be considered in nonimmunized children. Suspect anaerobes if foul-smelling discharge or necrosis is present or if there is a history of an animal or human bite. Consider a viral cause if preseptal cellulitis is associated with a vesicular skin rash (e.g., herpes simplex or varicella zoster).
Daily until clear and consistent improvement is demonstrated, then every 2 to 7 days until the condition has totally resolved. If preseptal cellulitis progresses despite antibiotic therapy, the patient is admitted to the hospital and a repeat (or initial) orbital CT scan is obtained. For patients already on p.o. antibiotics, switch to i.v. antibiotics (see 7.3.1, ORBITAL CELLULITIS).