The basic principle of corneal refractive surgery is to induce a change in the curvature of the cornea to correct a preexisting refractive error.
COMPLICATIONS OF SURFACE ABLATION PROCEDURES (PHOTOREFRACTIVE KERATECTOMY, LASER SUBEPITHELIAL KERATECTOMY, AND EPITHELIAL LASER IN SITU KERATOMILEUSIS)
In PRK, the corneal epithelium is removed and the corneal stroma is ablated using an argon–fluoride excimer laser (193 nm, ultraviolet) to correct a refractive error. In laser subepithelial keratomileusis (LASEK), the epithelium is chemically separated from the Bowman layer, moved to the side before laser ablation of the stroma, and then repositioned centrally. In epithelial laser in situ keratomileusis (epi-LASIK), the epithelium is mechanically separated from the Bowman layer, moved to the side before laser ablation of the stroma, and then repositioned centrally or discarded (see Table 4.31.1).
TABLE 4.31.1: Refractive Surgery Characteristics
| PRK | LASEK | Epi-LASIK | LASIK | SMILE | |
|---|---|---|---|---|---|
| Epithelial flap or method of stromal exposure | No flap. Epithelium removed by blade, spatula, brush, excimer laser, or dilute absolute alcohol. | Epithelial flap created by 20% absolute alcohol concentrated on epithelium by marker well. | Epithelial flap created by a blunt blade epi-keratome. Epithelial flap may be replaced (epi-on) or discarded (epi-off). | Epithelial and stromal flap created by sharp microkeratome or femtosecond laser. | No flap. Thin disc of stroma created by femtosecond laser and then mechanically extracted through small incision. |
| Depth of exposure | Bowman membrane | Bowman membrane | Bowman membrane | Anterior stroma (sub-Bowman keratomileusis provides more superficial stromal exposure) | Anterior stroma |
| Typical refractive limitations | Spherical range: −10.0D–+3.0D, cylinder range up to 3.0D | Spherical range: −8.0D–+3.0D, cylinder range up to 3.0D | Spherical range: −8.0D–+3.0D, cylinder range up to 3.0D | Spherical range: −10.0D–+3.0D, cylinder range up to 3.0D | Spherical range: −10.0D−1.0D, cylinder range up to 3.0D |
| Advantages | Useful in thin corneas, epithelial pathology. No stromal flap healing issues. | Useful in thin corneas, epithelial pathology. No stromal flap healing issues. | Useful in thin corneas, epithelial pathology. No stromal flap healing issues. | Minimal pain, rapid visual recovery, minimal stromal haze. | Minimal pain, rapid visual recovery. Minimal cap complications. Possibly less dry eye than LASIK. |
| Disadvantages | Postoperative pain, slower visual recovery, higher risk of subepithelial haze. | Postoperative pain, slower visual recovery, higher risk of subepithelial haze. | Postoperative pain, slower visual recovery, higher risk of subepithelial haze. Not ideal with significant glaucoma or anterior corneal scarring. | Not ideal for thin corneas, epithelial dystrophies, severe dry eyes, significant glaucoma. Presence of flap with possible complications (see text). | Currently only for myopia or myopic astigmatism in the US. Not ideal for thin corneas or in corneas with epithelial pathology. Removal of stromal lenticule can be technically difficult. SMILE enhancements complex; reoperations often done with PRK. |
Decreasing visual acuity and increased pain.
The induced epithelial defect at surgery, which usually takes a few days to heal, normally will cause postoperative pain. A bandage soft contact lens is used to minimize this discomfort. |
Later (2 Weeks to Several Months)
Decreasing visual acuity, severe glare, and monocular diplopia.
Corneal infiltrate and central corneal scar.
Dislocated or poorly fit bandage soft contact lens (see 4.21, Contact Lens–Related Problems).
Nonhealing epithelial defect (see 3.3, Corneal Abrasion). Must also consider HSV keratitis.
Corneal ulcer (see 4.12, Bacterial Keratitis).
Medication allergy (see 5.1, Acute Conjunctivitis).
Irregular astigmatism (e.g., central island, decentered ablation).
Steroid-induced glaucoma or ocular hypertension (see 9.8, Steroid-Response Glaucoma).
Complete ophthalmic examination, including IOP measurement. IOP may be underestimated given decreased corneal thickness.
Refraction if change in refractive error suspected. Hard contact lens overrefraction corrects irregular astigmatism.
Corneal topography and/or tomography if irregular astigmatism is suspected.
Epithelial defect (see 3.3, Corneal Abrasion).
Infectious keratitis (see 4.16, Herpes Simplex Keratitis and 4.12, Bacterial Keratitis).
Corneal haze: Increase steroid drop frequency. Follow up in 1 to 2 weeks. Cases of severe haze may respond to excimer laser PTK with mitomycin C.
Refractive error or irregular astigmatism: Consider surface ablation enhancement. If irregular astigmatism is present, hard contact lens, topography-guided surface ablation, or excimer laser PTK may be needed.
Steroid-induced glaucoma. See 9.8, Steroid-Response Glaucoma.
COMPLICATIONS OF LASER IN SITU KERATOMILEUSIS
In LASIK, a hinged, partial-thickness corneal flap is created using a microkeratome or femtosecond laser (1,053 nm, near-infrared), and then the underlying stroma is ablated with an excimer laser to correct refractive error. The corneal flap is repositioned over the stromal bed without sutures.
Decreasing visual acuity and increased pain.
Later (2 Weeks to Several Months)
Decreasing visual acuity, severe glare, monocular diplopia, and dry eye symptoms.
Severe conjunctival injection, corneal infiltrate, large fluorescein-staining epithelial defect, dislocated corneal flap, interface inflammation, epithelial ingrowth under the flap, central corneal scar, SPK, scissoring of the light reflex or retinoscopy, and irregular corneal thinning or steepening.
Dry eye/neurotrophic keratopathy. By far the most common early complication.
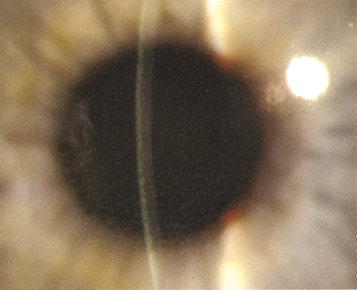
Diffuse lamellar keratitis (DLK). Also known as “sands of the Sahara” because of its appearance (multiple fine inflammatory infiltrates in the flap interface). Usually occurs within 5 days of surgery (see Figure 4.31.1).
Corneal ulcer and/or infection in flap interface. See 4.12, Bacterial Keratitis.
Central toxic keratopathy (CTK). Central corneal stromal opacification and consolidation of unknown etiology, causing corneal thinning and flattening. It tends to improve over 6 to 12 months.
Medication allergy. See 5.1, Acute Conjunctivitis.
Patients after LASIK have reduced corneal sensation in the area of the flap for at least 3 months (returns to essentially normal in 6 to 12 months). |
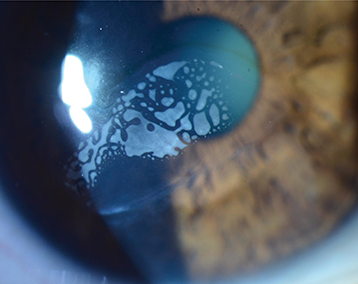
Epithelial ingrowth into flap interface (see Figure 4.31.2).
Corneal haze (scarring): Less common than after surface ablation procedures.
Irregular astigmatism (e.g., decentered ablation, central island, flap irregularity, ectasia).
DLK can occur weeks to years after LASIK in response to a corneal insult such as corneal abrasion, recurrent erosion, or viral keratitis.
Pressure-induced stromal keratitis (PISK). High IOP (often secondary to steroid response) can cause the development of fluid in the interface with a clinical appearance similar to DLK. IOP measurements are falsely low due to the fluid cleft, and pressure should be measured with a handheld tonometer (e.g., Tono-Pen or iCare) both on the central cornea and peripheral to the LASIK flap.
Complete slit-lamp examination, including fluorescein staining and IOP measurement by Tono-Pen and applanation. IOP may be underestimated given flap creation and decreased corneal thickness. Check IOP peripheral to the flap edge if PISK is suspected.
Refraction on all patients who do not have uncorrected vision of 20/20. Refraction with hard contact lens for irregular astigmatism.
Corneal topography and/or tomography for suspected irregular astigmatism.
Lost corneal flap: Treat as epithelial defect. See 3.3, Corneal Abrasion.
Epithelial defect. See 3.3, Corneal Abrasion.
SPK and dry eye. See 4.1, Superficial Punctate Keratopathy and 4.3, Dry Eye Syndrome.
DLK: Aggressive treatment with frequent topical steroids (e.g., prednisolone acetate 1% q1h). If severe, may also require lifting of flap and irrigation of interface. Treat any underlying cause, such as an epithelial defect.
PISK: Ocular hypotensive medications and rapid tapering of steroids.
Corneal infiltrate. See 4.12, Bacterial Keratitis and Appendix 8, Corneal Culture Procedure. The flap may need to be lifted to obtain the best culture results.
Epithelial ingrowth: Observation if very peripheral and not affecting vision. Surgical debridement with possible flap suturing if dense, affecting the health of flap, approaching visual axis, or affecting vision. Small pockets may also be treated with a YAG laser.
Corneal haze: Increase steroid drop frequency. Follow up in 1 to 2 weeks.
Refractive error or irregular astigmatism: Appropriate refraction. Consider PRK or LASIK enhancement. If irregular astigmatism, consider flap repositioning, custom or topography-guided enhancement, or hard contact lens fitting.
COMPLICATIONS OF SMALL INCISION LENTICULE EXTRACTION
In SMILE, a femtosecond laser is used to create a thin disc of tissue (lenticule) inside the corneal stroma, which is then mechanically dissected and extracted through a small peripheral incision.
Decreasing visual acuity and increased pain.
Later (2 weeks to Several Months)
Decreasing visual acuity, severe glare, monocular diplopia, and dry eye symptoms.
Severe conjunctival injection, corneal infiltrate, large epithelial defect, interface inflammation, epithelial ingrowth into interface, central corneal scar, scissoring of the light reflex or retinoscopy, and irregular corneal thinning or steepening.
DLK: Also known as “sands of the Sahara” because of its appearance (multiple fine inflammatory infiltrates in the interface). Usually occurs within 5 days of surgery.
Corneal ulcer and/or infection in interface. See 4.12, Bacterial Keratitis.
Medication allergy. See 5.1, Acute Conjunctivitis.
Early postoperative dry eye symptoms of SMILE are comparable to LASIK but often with faster recovery. Corneal denervation is also expected to be decreased compared with LASIK. |
Corneal haze (scarring): Less common than after surface ablation procedures.
Irregular astigmatism (e.g., retained lenticule fragments, decentered treatment, ectasia).
DLK can occur weeks to years after SMILE in response to a corneal insult such as corneal abrasion, recurrent erosion, or viral keratitis.
PISK: High IOP (often secondary to steroid response) can cause the development of fluid in the interface with a clinical appearance similar to DLK. IOP measurements are falsely low by the fluid cleft, and pressure should be measured with a handheld tonometer (e.g., Tono-Pen or iCare) both on the central cornea and peripheral to the SMILE cap.
Complete slit-lamp examination, including fluorescein staining and IOP measurement by Tono-Pen and applanation. IOP may be underestimated given lenticule extraction and decreased corneal thickness. Check IOP peripheral to the cap edge if PISK is suspected.
Refraction on all patients who do not have uncorrected vision of 20/20. Refraction with hard contact lens for irregular astigmatism.
Corneal topography and/or tomography for suspected irregular astigmatism.
Cap microstriae: Gentle cap massage, frequent topical steroids.
Epithelial defect. See 3.3, Corneal Abrasion.
SPK and dry eye. See 4.1, Superficial Punctate Keratopathy and 4.3, Dry Eye Syndrome.
DLK: Aggressive treatment with frequent topical steroids (e.g., prednisolone acetate 1% q1h). If severe, may also require lifting of flap and irrigation of interface. Treat any underlying cause, such as an epithelial defect.
PISK: Ocular hypotensive medications and rapid tapering of steroids.
Corneal infiltrate. See 4.12, Bacterial Keratitis and Appendix 8, Corneal Culture Procedure.
Epithelial ingrowth: Observation if very peripheral and not affecting vision. Attempt removal of cells through the small incision or consider conversion of cap into a flap and surgical debridement with possible suturing if dense, affecting the health of cap, approaching visual axis, or affecting vision. Small pockets can also be treated with a YAG laser.
Corneal haze: Increase steroid drop frequency. Follow up in 1 to 2 weeks.
Refractive error or irregular astigmatism: Appropriate refraction. Consider PRK enhancement. If irregular astigmatism, consider custom or topography-guided enhancement or hard contact lens fitting.
COMPLICATIONS OF RADIAL KERATOTOMY
In radial keratotomy (RK), partial-thickness, spoke-like cuts are made in the peripheral cornea using a diamond blade (often 90% to 95% depth), which results in a flattening of the central cornea and correction of myopia. Astigmatic keratotomy (AK) is a similar procedure in which arcuate or tangential relaxing incisions are made to correct astigmatism. Now rarely used given complication rate and advancement of technology.
Decreasing visual acuity and increased pain.
Decreasing visual acuity, severe glare, and monocular diplopia.
Corneal infiltrate, large fluorescein-staining epithelial defect, rupture at RK incision site after trauma, and anterior chamber reaction.
Large epithelial defect. See 3.3, Corneal Abrasion.
Corneal ulcer/infection in RK incision. See 4.12, Bacterial Keratitis.
Medication allergy. See 5.1, Acute Conjunctivitis.
Very rarely, endophthalmitis. See 12.14, Acute Postoperative Endophthalmitis and 12.15, Subacute and Chronic Postoperative Uveitis.
RK incisions approaching the visual axis causing glare and starbursts.
Regression of refractive error; common in first few months after surgery.
Progression of refractive effect (consecutive hyperopia); common after first few years after surgery.
Ruptured globe at RK incision site after trauma. See 3.10, Ruptured Globe and Penetrating Ocular Injury.
Complete slit-lamp examination, including IOP measurement and fluorescein staining.
Refraction on all patients who do not have uncorrected vision of 20/20. Refraction with hard contact lens for irregular astigmatism.
Corneal topography and/or tomography if irregular astigmatism suspected.
Corneal infiltrate: See 4.12, Bacterial Keratitis and Appendix 8, Corneal Culture Procedure.
Epithelial defect: See 3.3, Corneal Abrasion.
Endophthalmitis: See 12.14, Acute Postoperative Endophthalmitis and 12.15, Subacute and Chronic Postoperative Uveitis.
Refractive error or irregular astigmatism: Appropriate refraction. Consider enhancement of RK incisions or AK. Rarely, surface laser ablation with mitomycin C can be used. Irregular astigmatism may require a hard contact lens.
Ruptured globe at RK incision: Requires surgical repair. See 3.10, Ruptured Globe and Penetrating Ocular Injury.