Double vision, eyelid droop, pain in the distribution of the V-1 and V-2 branches of the ipsilateral trigeminal nerve, or numbness.
Critical
Limitation of eye movement corresponding to any combination of a third, fourth, or sixth cranial nerve palsy on one side; facial pain or numbness or both corresponding to first or second branches of the fifth cranial nerve; ptosis and a small pupil (Horner syndrome); the pupil also may be dilated if the third cranial nerve is involved. Any combination of the above may be present simultaneously because of the anatomy of the cavernous sinus. All signs involve the same side of the face when one cavernous sinus/superior orbital fissure is involved. The circular sinus connects the cavernous sinuses, and its involvement can cause contralateral signs. Consider orbital apex syndrome when proptosis and optic neuropathy are present.
Other
Proptosis may be present when the superior orbital fissure is involved.
Myasthenia gravis: Fatigable ptosis, orbicularis weakness, and limited motility. Pupils never involved and never any sensory symptoms. No proptosis. See 10.11, Myasthenia Gravis.
CPEO: Progressive, painless, bilateral motility limitation with ptosis. Normal pupils. Orbicularis always weak. See 10.12, Chronic Progressive External Ophthalmoplegia.
Orbital lesions (e.g., tumor, thyroid disease, inflammation). Proptosis and increased resistance to retropulsion are usually present, in addition to motility restriction. Results of forced duction tests are abnormal (see Appendix 6, Forced Duction Test and Active Force Generation Test). May have an afferent pupillary defect if the optic nerve is involved.
|
 NOTE NOTEOrbital apex syndrome combines the superior orbital fissure syndrome with optic nerve dysfunction, and most commonly results from an orbital lesion. |
Brainstem disease: Tumors and vascular lesions of the brainstem produce ocular motor nerve palsies, particularly the sixth cranial nerve. MRI of the posterior fossa and brainstem is best for making this diagnosis.
Carcinomatous meningitis: Diffuse seeding and infiltration of the leptomeninges by metastatic tumor cells can produce a rapidly sequential bilateral cranial nerve disorder. Workup includes neuroimaging and LP.
Skull base tumors, especially nasopharyngeal carcinoma or clivus lesions: Most commonly affects the sixth cranial nerve, but the second, third, fourth, and fifth cranial nerves may be involved as well. Typically, one cranial nerve after another is affected by invasion of the skull base. The patient may have cervical lymphadenopathy, nasal obstruction, ear pain, or popping caused by serous otitis media or blockage of the Eustachian tube, weight loss, or proptosis.
Clivus tumors may produce fluctuating symptoms of double vision with an incomitant esotropia and only very mildly limited abduction deficits. These tumors also may produce relatively comitant esotropias due to involvement of both sixth cranial nerves as they ascend the clivus.
Progressive supranuclear palsy (PSP): Vertical limitation of eye movements, typically beginning with downward gaze. Postural instability, dementia, and rigidity of the neck and trunk may be present. All eye movements are eventually lost. Significant cognitive impairment is often present and can progress rapidly. See 10.12, Chronic Progressive External Ophthalmoplegia.
Rare: Myotonic dystrophy, bulbar variant of the Guillain–Barré syndrome (Miller–Fisher variant), intracranial sarcoidosis, others.
History: Diabetes? Hypertension? Recent significant head trauma? Prior cancer (including skin cancer)? Weight loss? Ocular bruit? Recent infection? Severe headache? Diurnal variation of symptoms?
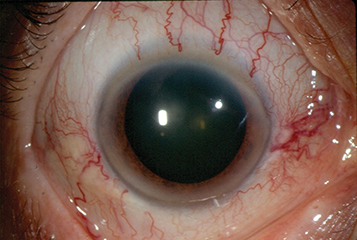
Ophthalmic examination: Careful attention to pupils, extraocular motility, Hertel exophthalmometry, and resistance to retropulsion. May see corkscrew conjunctival vessels (see Figure 10.10.1).
Examine the periocular skin for malignant or locally invasive lesions.
CT scan (axial, coronal, and parasagittal views) or MRI of the sinuses, orbit, and brain.
Orbital color Doppler imaging is a dynamic evaluation, distinct from the static images of CT, MRI, and MRA. It is quick, painless, noninvasive and may be diagnostic when the other imaging studies are unrevealing. For some AVMs and carotid-cavernous fistulas, cerebral angiography is required for diagnosis, and often for treatment.
LP to rule out carcinomatous meningitis in patients with a history of primary carcinoma. More than one LP might be required in some cases.
Nasopharyngeal examination with or without a biopsy to rule out nasopharyngeal carcinoma or infectious process.
Lymph node biopsy when lymphadenopathy is present.
CBC with differential, ESR, ANA, rheumatoid factor to rule out infection, malignancy, and systemic vasculitis. Antineutrophilic cytoplasmic antibody if granulomatosis with polyangiitis is suspected.
|
 NOTE NOTEPatients suspected of having dural AVFs are recommended to undergo cerebral angiography to look for cortical venous drainage. If present, this puts the patient at greater risk for intracranial hemorrhage. These AVMs may present with a variable double vision syndrome involving partial paresis of the third, fourth and sixth cranial nerves. These lesions do not produce proptosis or any of the other external signs of cavernous sinus vascular lesions. The eyes are white and quiet. These lesions are especially difficult to diagnose and can produce large stroke syndromes. |
If cavernous sinus thrombosis is considered, obtain two to three sets of peripheral blood cultures and also culture the presumed primary source of the infection. Lemierre syndrome refers to an infectious thrombophlebitis of the internal jugular vein that is a result of spread from an oropharyngeal infection. This rare and potentially fatal entity may present in young, otherwise healthy individuals with neck pain, signs of sepsis, proptosis, and extraocular motility deficits.
Treatment and Follow-Up
Arteriovenous Fistula
Many dural fistulas close spontaneously or after cerebral angiography. Others may require treatment via interventional neuroradiologic techniques.
Resolution of the fistula usually results in normalization of the intraocular pressure. However, medical treatment with aqueous suppressants for secondary glaucoma may be necessary. Drugs that increase outflow facility (e.g., latanoprost and pilocarpine) are usually not as effective because the intraocular pressure is increased as a result of increased episcleral venous pressure. See 9.1, Primary Open-Angle Glaucoma.
Metastatic Disease to the Cavernous Sinus
Often requires systemic chemotherapy (if a primary is found) with or without radiation therapy to the metastasis. Refer to an oncologist.
Intracavernous Aneurysm
Refer to a neurosurgeon for workup and possible treatment.
Zygomycosis (Mucormycosis)
Immediate hospitalization because this is a rapidly progressive, life-threatening disease.
Emergent CT scan of the sinuses, orbit, and brain.
Consult infectious disease, neurosurgery, otolaryngology, and endocrinology as indicated.
Begin amphotericin B 0.25 to 0.30 mg/kg i.v. in D
5W slowly over 3 to 6 hours on the first day, 0.5 mg/kg i.v. on the second day, and then up to 0.8 to 1.0 mg/kg i.v. daily. The duration of treatment is determined by the clinical condition.
|
 NOTE NOTERenal status and electrolytes must be checked before initiating therapy with amphotericin B and then monitored closely during treatment. Liposomal amphotericin has significantly less renal toxicity. |
A biopsy should be obtained from any necrotic tissue (e.g., nasopharynx, paranasal sinuses) if zygomycosis/mucormycosis is suspected.
Early surgical debridement of all necrotic tissue (possibly including orbital exenteration), plus irrigation of the involved areas with amphotericin B, is often necessary to eradicate the infection.
Treat the underlying medical condition (e.g., diabetic ketoacidosis), with appropriate consultation as required.
Pituitary Apoplexy
These patients may be quite ill and require immediate systemic steroid therapy. Refer emergently to neurosurgery for surgical consideration.
Varicella Zoster Virus
See 4.17, Herpes Zoster Ophthalmicus/Varicella Zoster Virus.
Cavernous Sinus Thrombosis
For possible infectious cases (usually caused by Staphylococcus aureus), hospitalize the patient for treatment with intravenous antibiotics for several weeks. Consult infectious disease for antibiotic management.
Intravenous fluid replacement is usually required.
For aseptic cavernous sinus thrombosis, consider systemic anticoagulation (heparin followed by warfarin) or aspirin 325 mg p.o. daily in collaboration with a medical internist.
Exposure keratopathy is treated with preservative-free lubricating ointment or drops (see 4.5, Exposure Keratopathy).
Treat secondary glaucoma. See 9.1, Primary Open-Angle Glaucoma.
Tolosa–Hunt Syndrome
Prednisone 80 to 100 mg p.o. daily for 1 week, and then decrease dose by 10 mg per week until discontinued. If pain persists after 72 hours, stop steroids and initiate reinvestigation to rule out other disorders. This condition requires a very gradual steroid taper.
|
 NOTE NOTEOther infectious or inflammatory disorders may also respond to steroids initially, so these patients need to be monitored closely. |