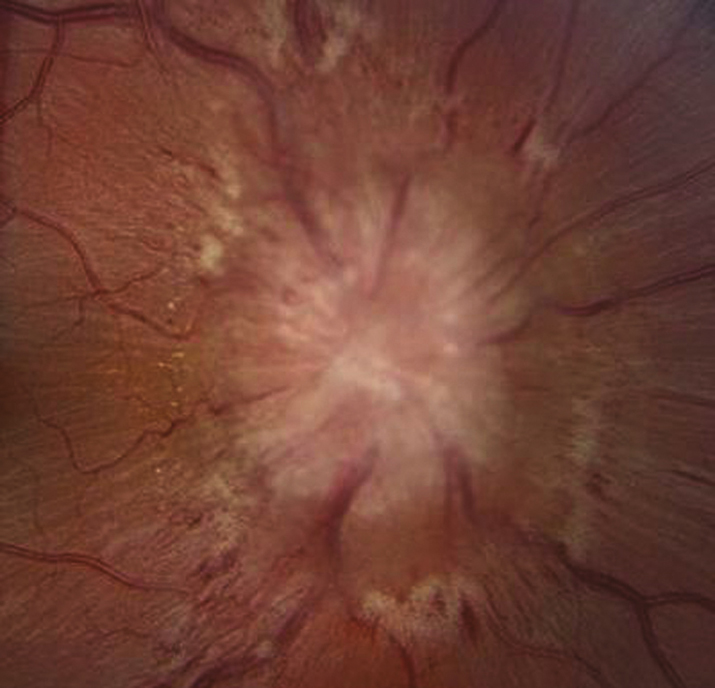
(See Figure 10.15.1.)
Critical
Bilaterally swollen, hyperemic discs (in early papilledema, disc swelling may be asymmetric) with nerve fiber layer edema causing blurring of the disc margin, often obscuring the blood vessels.
Other
Papillary or peripapillary retinal hemorrhages (often flame shaped); loss of venous pulsations (20% of the normal population do not have venous pulsations); dilated, tortuous retinal veins; normal pupillary response and color vision; an enlarged physiologic blind spot or other visual field defects by formal visual field testing.
In chronic papilledema, the hemorrhages and cotton–wool spots resolve, disc hyperemia disappears, and the disc becomes gray in color. Peripapillary gliosis and narrowing of the peripapillary retinal vessels occur, and optociliary shunt vessels may develop on the disc. Loss of color vision, loss of central visual acuity, and visual field defects (especially inferonasally) may be observed.
Unilateral or bilateral sixth cranial nerve palsy may result from increased intracranial pressure. |