Definition
Optic disc swelling produced by increased intracranial pressure.
Episodes of transient, usually bilateral visual loss (lasting seconds), often precipitated after rising from a lying or sitting position (altering intracranial pressure); headache; double vision; nausea; vomiting; and, rarely, a decrease in visual acuity (a mild decrease in visual acuity can occur in the acute setting if associated with a macular disturbance). Visual field defects and severe loss of central visual acuity occur more often with chronic papilledema.
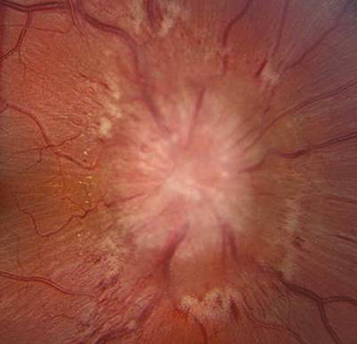
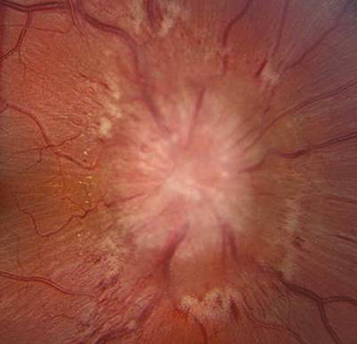
(See Figure 10.15.1.)
Figure 10.15.1: Swollen optic disc with obscured blood vessels and blurring of the disc margin.
Flame-shaped hemorrhages may occur.
Critical
Bilaterally swollen, hyperemic discs (in early papilledema, disc swelling may be asymmetric) with nerve fiber layer edema causing blurring of the disc margin, often obscuring the blood vessels.
Other
Papillary or peripapillary retinal hemorrhages (often flame shaped); loss of venous pulsations (20% of the normal population do not have venous pulsations); dilated, tortuous retinal veins; normal pupillary response and color vision; an enlarged physiologic blind spot, nasal or other visual field defects by formal visual field testing.
In chronic papilledema, the hemorrhages and cotton–wool spots resolve, disc hyperemia disappears, and the disc becomes gray in color. Peripapillary gliosis and narrowing of the peripapillary retinal vessels occur, and optociliary shunt vessels may develop on the disc. Loss of color vision, loss of central visual acuity, and advanced visual field defects depending on the severity and duration of papilledema (especially nasally) may be observed.
|
 NOTE NOTEUnilateral or bilateral sixth cranial nerve palsy may result from increased intracranial pressure. |
Differential Diagnosis of Disc Edema or Elevation
Pseudopapilledema (e.g., optic disc drusen or congenitally anomalous disc): Not true disc swelling. Vessels overlying the disc are not obscured, the disc is not hyperemic, and the surrounding nerve fiber layer is normal. Spontaneous venous pulsations (SVPs) are often present. Buried drusen may be present and can be identified with B-scan ultrasound (US) or autofluorescence; will also be visible on CT imaging.
Papillitis: An afferent pupillary defect and decreased color vision are present; decreased visual acuity occurs in most cases, usually unilateral. See 10.14, Optic Neuritis.
Hypertensive optic neuropathy: Extremely high blood pressure, narrowed arterioles, arteriovenous crossing changes, hemorrhages with or without cotton–wool spots extending into the peripheral retina. See 11.10, Hypertensive Retinopathy.
Central retinal vein occlusion: Hemorrhages extend far beyond the peripapillary area; dilated and tortuous veins, generally unilateral; acute loss of vision in most cases. See 11.8, Central Retinal Vein Occlusion.
Ischemic optic neuropathy: Disc swelling is pale but may be hyperemic; initially unilateral unless due to GCA, with sudden visual loss. See 10.17, Arteritic Ischemic Optic Neuropathy (Giant Cell Arteritis) and 10.18, Nonarteritic Ischemic Optic Neuropathy.
Infiltration of the optic disc (e.g., sarcoid or tuberculous granuloma, leukemia, metastasis, other inflammatory disease or tumor): Other ocular or systemic abnormalities may be present. Usually unilateral.
Leber hereditary optic neuropathy: Usually occurs in males in the second or third decade of life. Patients may have a family history and present with rapid visual loss of one and then the other eye within days to months. Early examination of the disc may reveal peripapillary telangiectasias followed by optic atrophy.
Orbital optic nerve tumors: Unilateral disc swelling, may have proptosis.
Diabetic papillopathy: Benign disc edema in one or both eyes of a diabetic patient, most commonly with mild visual loss. No correlation with diabetic retinopathy. In addition to disc edema, disc hyperemia due to telangiectasias of the disc vessels may occur, simulating neovascularization. More common in patients with juvenile-onset diabetes. No treatment is indicated. Spontaneous resolution usually occurs after 3 to 4 months but may take even longer.
Thyroid-related optic neuropathy: May have eyelid lag or retraction, ocular misalignment, resistance to retropulsion. See 7.2.1, Thyroid Eye Disease.
Uveitis (e.g., syphilis or sarcoidosis): Pain or photophobia, anterior chamber/vitreous cells. See 12.3, Posterior Uveitis.
Amiodarone toxicity: May present with subacute bilateral asymmetric/symmetric visual loss and disc edema.
|
 NOTE NOTEOptic disc swelling in a patient with leukemia is often a sign of leukemic optic nerve infiltration. Urgent initiation of therapy including corticosteroids and chemotherapy/radiation is required to achieve best visual outcomes. |
Treatment should be directed at the underlying cause of the increased intracranial pressure.