CMV is the most frequent ocular opportunistic infection in patients with AIDS, but is 80% to 90% less common in the era of ART. CMV is almost never seen unless the CD4+ count is <100 cells/mm3. Because active retinitis is often asymptomatic, patients with CD4+ counts <100 cells/mm3 should be seen at least every 3 to 6 months. May also be seen in other immunocompromised states (e.g., leukemia and post-transplant patients). Local ocular immunosuppression (intraocular and periocular steroid injections) may precipitate CMV retinitis in otherwise healthy patients.
Scotoma or decreased vision in one or both eyes, floaters, or photopsias. Pain and photophobia are uncommon. Often asymptomatic.
Critical
Indolent form: Peripheral granular opacities with or without hemorrhage. The absence of hemorrhage does not rule out CMV retinitis.
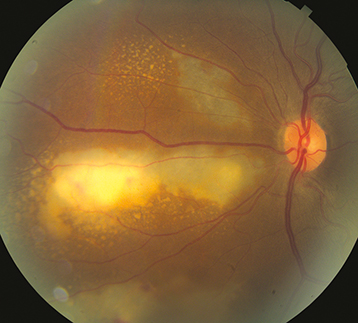
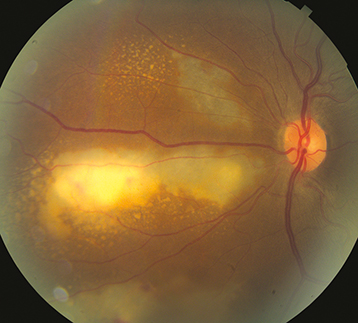
Fulminant form: Confluent areas of necrosis with prominent intraretinal hemorrhage, with perivascular infiltration along the major retinal vascular arcades. Progressive retinal atrophy may also indicate active CMV (See Figure 12.12.1).
Figure 12.12.1: CMV retinitis.
Frosted branch angiitis form: Profound retinal vasculitis with severe vascular exudating affecting both the arterioles and venules.
Other
Anterior uveitis with nongranulomatous, stellate KP almost always present but mild. Vitritis is usually mild. RPE atrophy and pigment clumping result once the active process resolves. Rhegmatogenous retinal detachment (RRD) occurs in approximately one-third of patients with CMV retinitis with increased risk when >25% of the retina is involved.
The following conditions may closely simulate CMV retinitis.
ARN. See 12.13, Acute Retinal Necrosis(see Table 12.12.1).
TABLE 12.12.1: Cytomegalovirus (CMV) Retinitis Versus Acute Retinal Necrosis (ARN) Versus Progressive Outer Retinal Necrosis (PORN) Versus Toxoplasmosis
| CMV | ARN | PORN | Toxoplasmosis |
|---|
| Retinal hemorrhages | Common | Uncommon | Uncommon | Usually absent |
| Vitritis | Minimal | Significant | Absent | Significant |
| Pain | Absent | Variable | Absent | Moderate |
| Immune status | Immunocompromised | Usually healthy | Immunocompromised | Either |
| Appearance | (1) Granular retinitis has a “Brushfire” border with the leading edge of active granular retinitis and mottled RPE in its wake; (2) Fulminant retinitis has a “pizza pie” appearance with larger swaths of retinitis and prominent hemorrhage; (3) Frosted branch angiitis | Sharply demarcated lesions with a nearly homogeneous appearance | Multifocal patches of deep retinal necrosis, rapid progression with the involvement of the macula | “Headlight in the fog” with dense vitritis and smooth edges; adjacent to a pigmented chorioretinal scar if reactivation |
Syphilis. See 12.10, Syphilis.
HIV retinopathy. See 12.11, HIV Retinopathy.
Toxoplasmosis. See 12.9, Toxoplasmosis.
See Table 12.12.2 for treatment details.
TABLE 12.12.2: Therapy for CMV Retinitis
| Drug | Induction Dose | Maintenance Dose | Toxicities | Contraindications |
|---|
| Ganciclovira | 5 mg/kg i.v. b.i.d. for 14 days | 5 mg/kg i.v. daily | Neutropenia, thrombocytopenia, anemia | Absolute neutrophil count <500/mm3, platelets <25,000/mm3; Potentially embryotoxic |
| Valganciclovirb | 900 mg p.o. b.i.d. for 21 days | 900 mg p.o. daily | Neutropenia, thrombocytopenia, anemia | Absolute neutrophil count <500/mm3, platelets <25,000/mm3; Potentially embryotoxic |
| Foscarnet | 90 mg/kg i.v. b.i.d. for 14 days | 90 to 120 mg/kg i.v. dailyc | Renal impairment neutropenia, anemia, electrolyte imbalances | Use caution with renal impairment or electrolyte imbalances |
| Cidofovir | 5 mg/kg i.v. weekly for 3 wk | 3 to 5 mg/kg i.v. every 2 wk | Dose- and schedule-dependent nephrotoxicity, hypotony (necessitates discontinuation), uveitis (steroid responsive); Must be given with probenecid | Recurrent uveitis, moderate to severe kidney disease, intolerance to probenecid |
a Compared with intravitreal therapy alone, there is a decreased risk of mortality (50%), systemic disease (90%), and fellow eye involvement (80%) in patients treated with concomitant systemic anti-CMV therapy. Moreover, the risk of retinitis progression is significantly greater in eyes treated with intravitreal therapy alone.
b Compared with i.v. ganciclovir, there is an increased risk of systemic disease (30%) and fellow eye involvement (50%) after 6 months. However, the relapse-free interval is greatly increased.
c During the induction phase, 500 mL of normal saline is used for each dose. During maintenance, 1000 mL of saline should be used.
Oral therapy with valganciclovir 900 mg p.o. b.i.d. for induction (21 days), followed by 900 mg p.o. daily for maintenance. Alternatively, intravenous ganciclovir 5 mg/kg b.i.d. or foscarnet 90 mg/kg b.i.d. (adjusting for renal function) may be used, followed by oral therapy valganciclovir (900 mg p.o. b.i.d. to complete 3-week induction, then 900 mg p.o. daily). The goal of treatment is quiescent retinitis (nonprogressive areas of RPE atrophy with a stable opacified border). Patients with progression of retinitis despite induction or who have disease that threatens the macula or optic nerve head may benefit from intravitreal antiviral injections (foscarnet 2.4 mg/0.1 mL or ganciclovir 4 mg/0.1 mL), but systemic therapy is still necessary to prevent the involvement of the fellow eye.
Under the direction of an internist or infectious disease specialist, ART should be initiated or optimized; immune recovery with sustained CD4+ counts >200 cells/mm3 results in decreased risk of retinal detachment, second-eye involvement, antiviral resistance, and mortality. Also, monitor for toxicity of anti-CMV therapy (valganciclovir and ganciclovir cause bone marrow toxicity; foscarnet is nephrotoxic and can cause electrolyte abnormalities and seizures; intravenous ganciclovir and foscarnet require placement of an indwelling catheter, which may cause line infection and sepsis).
Small, macula-sparing RRDs may be treated with laser demarcation, but multiple retinal breaks are typical and may be missed; pars plana vitrectomy with silicone oil is indicated for most detachments, especially those involving the macula.
Primary prophylaxis (prevention of CMV retinitis) with oral valganciclovir in high-risk patients is usually not recommended because of potential toxicity except in transplant patients.
Ganciclovir resistance (reflected by positive blood or urine CMV cultures) may occur with prolonged treatment.
Complete blood count should be checked periodically due to myelosuppressive effects of valganciclovir and ganciclovir, especially in HIV patients.
All currently available anti-CMV therapy is virostatic, not virocidal, and almost all patients eventually relapse if not treated with ART. Serial fundus photographs are helpful for monitoring progression.
Relapse is defined as recurrent or new retinitis, movement of opacified border, or expansion of the atrophic zone.
Relapse can occur from resistance or subtherapeutic intraocular drug levels. Reinduction with the same medication is the first line of treatment.
Clinical resistance is defined as persistent or progressive retinitis despite induction-level medication for 6 weeks. Laboratory confirmation is possible for low-grade UL97 (viral phosphotransferase) or high-grade UL54 (viral DNA polymerase) mutations.
If resistance is recognized, a change in therapy from one antiviral to the other is indicated. Consider intravenous cidofovir 5 mg/kg once weekly for 2 weeks and then 3 to 5 mg/kg every 2 weeks. Cidofovir itself may cause uveitis and renal impairment and must be given with probenecid to reduce the nephrotoxicity. Intravitreal cidofovir is contraindicated because of the high risk of uveitis and hypotony. Cross-resistance can occur since all three anti-CMV drugs are CMV DNA polymerase inhibitors.
Discontinuation of anti-CMV maintenance therapy may be considered in select patients receiving highly active ART who have CD4+ counts >100 to 150 cells/mm3 for greater than 6 months and completely quiescent CMV retinitis. In these patients, whose immune system can control CMV, stopping maintenance therapy may prevent drug toxicity and drug-resistant organisms. In iatrogenically immunosuppressed patients, cessation or reduction in dosage of immunosuppressive drugs may be required for long-term control of CMV retinitis.
Immune recovery uveitis: Occurs in previously immunocompromised patients (HIV/iatrogenic) with CMV after the CD4+ count or immune system reconstitutes. In the presence of a functioning immune system, the CMV antigens elicit an inflammatory response that is predominantly posterior (e.g., vitritis, papillitis, CME, and ERM). Treatment may require topical, periocular, or intraocular steroids. Antivirals should be continued to avoid reactivation of CMV in cases of borderline CD4+ counts.