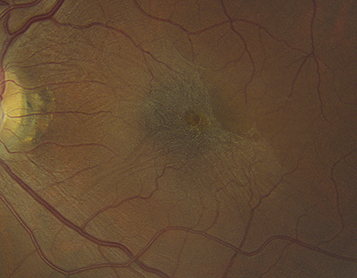
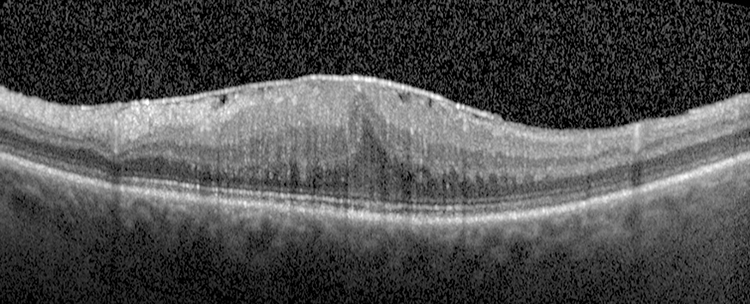
(See Figure 11.26.1.)
Spectrum ranges from a fine, glistening membrane (cellophane maculopathy) to a thick, gray-white membrane (macular pucker) present on the surface of the retina in the macular area.
Retinal folds radiating out from the membrane; displacement, straightening, or tortuosity of the macular retinal vessels; ME or macular detachment. A ring-shaped condensation of the ERM around the fovea may simulate a macular hole (pseudohole).