Tearing, irritation, pain, mild-to-severe photophobia. History of similar episodes or chalazia. Corneal phlyctenules are more symptomatic than conjunctival phlyctenules.
Critical
Conjunctival phlyctenule: A small, rounded, white inflammatory nodule on the bulbar conjunctiva, often at or near the limbus, in the center of a hyperemic area.
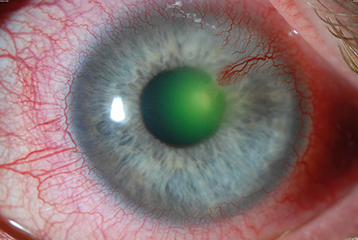
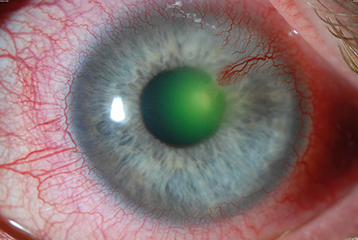
Corneal phlyctenule: A small, white nodule, initially near the limbus, with dilated conjunctival blood vessels approaching it. Often associated with epithelial ulceration and central corneal migration, producing wedge-shaped corneal neovascularization and scarring behind the leading edge of the lesion. Can be bilateral and recurrent (see Figure 4.20.1).
Figure 4.20.1: Corneal phlyctenule.
Other
Conjunctival injection, blepharitis, corneal scarring.
Delayed hypersensitivity reaction usually as a result of one of the following:
Staphylococcus: Usually related to blepharitis. See 4.19, Staphylococcal Hypersensitivity.
Rarely TB or another infectious agent (e.g., Coccidiomycosis, Candidiasis, lymphogranuloma venereum).
Indicated for symptomatic patients.
Topical steroid (e.g., loteprednol 0.5% or prednisolone acetate 1% q.i.d., depending on the severity of symptoms). A combination antibiotic/steroid can also be used q.i.d. (e.g., loteprednol 0.5%/tobramycin 0.3% or dexamethasone 0.1%/tobramycin 0.3%).
Topical ophthalmic antibiotic regimen in the presence of corneal ulcer. See 4.12, Bacterial Keratitis. Otherwise, antibiotic ointment (e.g., erythromycin, bacitracin) q.h.s.
Eyelid hygiene b.i.d. to t.i.d. for blepharitis. See 5.8, Blepharitis/Meibomitis.
Preservative-free artificial tears four to six times per day.
In severe cases of blepharitis or acne rosacea, consider doxycycline 50 to 100 mg p.o. daily to b.i.d., or erythromycin 200 mg p.o. daily to b.i.d. See 5.8, Blepharitis/Meibomitis.
If the PPD, IGRA, or chest radiograph is positive for TB, refer the patient to an internist or infectious disease specialist for management.
Recheck in several days to a week. Healing usually occurs over a 10- to 14-day period, with a residual stromal scar. When the symptoms have significantly improved, slowly taper the steroid. Maintain the antibiotic ointment and eyelid hygiene indefinitely. Continue oral antibiotics for 3 to 6 months at a lower daily dose (e.g., doxycycline 50 mg p.o. daily). Topical cyclosporine may be a beneficial steroid-sparing agent in patients with recurrent inflammation.