CHF may result from systolic “pump” dysfunction, increased LV diastolic “stiffness,” and/or acute mechanical complications.
Symptoms Dyspnea, orthopnea, tachycardia.
Examination Jugular venous distention, S3 and S4 gallop, pulmonary rales; systolic murmur if acute mitral regurgitation or ventricular septal defect (VSD) has developed.
Treatment: Heart Failure Initial therapy includes diuretics (begin with furosemide 10-20 mg IV), inhaled O2, and vasodilators, particularly nitrates (PO, topical, or IV [Chap. 124. Heart Failure and Cor Pulmonale] unless pt is hypotensive [systolic bp <100 mmHg]); digitalis is usually of little benefit in acute MI (See Chaps. 13. Acute Pulmonary Edema and 124. Heart Failure and Cor Pulmonale). Diuretic, vasodilator, and inotropic therapy (Table 119-1) may be guided by invasive hemodynamic monitoring (Swan-Ganz pulmonary artery catheter, arterial line), particularly in pts with accompanying hypotension (Table 119-2; Fig. 119-3). In acute MI, an acceptable pulmonary capillary wedge (PCW) pressure is 15-20 mmHg; in the absence of hypotension, PCW >20 mmHg is treated with diuretic plus vasodilator therapy (IV nitroglycerin [begin at 10 µg/min] or nitroprusside [begin at 0.5 µg/kg per min]) and titrated to optimize bp, PCW, and systemic vascular resistance (SVR). 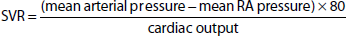 Normal SVR = 900 - 1350 dyne • s/cm5. If PCW >20 mmHg and pt is hypotensive (Table 119-2 and Fig. 119-3), evaluate for VSD or acute mitral regurgitation, consider dobutamine (begin at 1-2 [µg/kg]/min), titrate upward to maximum of 10 (µg/kg)/min; beware of drug-induced tachycardia or ventricular ectopy. After stabilization on parenteral vasodilator therapy, oral therapy follows with an ACE inhibitor or an ARB (Chap. 124. Heart Failure and Cor Pulmonale). Consider addition of long-term aldosterone antagonist (spironolactone 25-50 mg daily or eplerenone 25-50 mg daily) to ACE inhibitor if LVEF ≤40% or symptomatic heart failure or diabetes are present—do not use if renal insufficiency or hyperkalemia are present. |