Visualizes heart in real time with ultrasound; Doppler recordings noninvasively assess hemodynamics and abnormal flow patterns (Table 112-1 and Fig. 112-1). Imaging may be compromised in pts with chronic obstructive lung disease, thick chest wall, or narrow intercostal spaces.
Chamber Size and Ventricular Performance 
Assessment of atrial and ventricular dimensions, global and regional systolic wall motion abnormalities, ventricular hypertrophy/infiltration, evaluation for pulmonary hypertension: RV systolic pressure (RVSP) is calculated from maximum velocity of tricuspid regurgitation (TR):
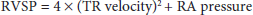
(RA pressure is same as JVP estimated by physical examination.) In absence of RV outflow obstruction, RVSP = pulmonary artery systolic pressure.
LV diastolic function is assessed by transmitral Doppler (see Fig. 270e-8, in HPIM-19) and Doppler tissue imaging, which measures velocity of myocardial relaxation.
Thickness, mobility, calcification, and regurgitation of each cardiac valve can be assessed. Severity of valvular stenosis is calculated by Doppler [peak gradient = 4 × (peak velocity)2]. Structural lesions (e.g., flail leaflet, vegetation) resulting in regurgitation may be identified, and Doppler (Fig. 112-2) estimates severity of regurgitation.
Echo is noninvasive modality of choice to rapidly identify pericardial effusion and assess its hemodynamic significance; in tamponade there is diastolic RA and RV collapse, dilatation of IVC, exaggerated respiratory alterations in transvalvular Doppler velocities. Actual thickness of pericardium (e.g., in suspected constrictive pericarditis) is better measured by CT or MRI.
May visualize atrial or ventricular thrombus, intracardiac tumors, and valvular vegetations. Yield of identifying cardiac source of embolism is low in the absence of cardiac history or physical findings. Transesophageal echocardiography (TEE) is more sensitive than standard transthoracic study for masses <1 cm in diameter.
Aneurysm and dissection of the aorta may be evaluated and complications (aortic regurgitation, tamponade) assessed (Chap. 125. Diseases of the Aorta) by standard transthoracic echo. TEE is more sensitive and specific for aortic dissection.
Echo, Doppler, and IV saline contrast echo are useful to identify congenital lesions and shunts (See Chap. 113. Congenital Heart Disease in the Adult).
Echo performed prior to, and after, treadmill or bicycle exercise identifies regions of prior MI and inducible myocardial ischemia (↓ regional contraction with exercise). Dobutamine pharmacologic stress echo can be substituted for pts who cannot exercise.
Outline